Click to download a PDF of this report.
Coauthored by Noor Chadha, Bernadette Lim, Madeleine Kane, and Brenly Rowland
(This report is also available on the website of the Institute for Healing and Justice in Medicine)
The use of biological race in medicine is an unchallenged, outdated norm throughout clinical education, research, and practice. Medicine largely frames racial health disparities in terms of biological difference and individual behavior, despite evidence that social and structural factors generate and perpetuate most health issues. As a result, medicine fails to address racism and its health consequences. This is bad and irresponsible science.
Racism—a structure and ideology that oppresses and limits resources to minority groups—is rarely discussed in clinical health and the health sciences as a meaningful determinant of health outcomes. Thus, racial health disparities are often wrongly attributed to biology and physiology of racial groups rather than the stratified socioeconomic opportunities that are available.
As medical students and graduate student researchers, we witness these harms every day in our textbooks, classrooms, clinics, and communities. We envision a world where the social construct of race is not conflated with biology and the health consequences of racism are acknowledged, addressed, and cared for in all their forms.
Acknowledgments
Interdisciplinary faculty editors and advisors
- Tina Sacks, PhD
- Osagie Obasogie, JD, PhD
- Amy Garlin, MD
- Monica Hahn, MD, MS, MPH
- Seth Holmes, MD, PhD
Interdisciplinary cosponsors
- University of California, Berkeley—Othering & Belonging Institute
- University of California, Berkeley—Center for Race & Gender Studies
Peer editors and peer contributors for our initial drafts
- Rachel Bigley
- James Cevallos
- Nicole Carvajal
- Willow Frye
- Nazineen Kandahari
- Interpreet Kaur
- Aminta Kouyate
- Sharada Narayan
- Luke Silverman-Lloyd
- Scott Swartz
- Nathan Swetlitz
- Shreya Thatai
- Kay Walker
Contents
- Why We Wrote This
- Executive Summary
- Introduction
- Section 1: Racism, Not Race, Causes Health Disparities
- Section 2: Cranial Capacities to Eugenics: How Medicine and Health Sciences Biologize Race
- Section 3: Race-Based Medicine in Diagnosis and Treatment
- Section 4: Looking Ahead
- Bibliography
- Appendix: For Further Reading
Why We Wrote This
We are students of medicine and public health at the Joint Medical Program of the University of California, San Francisco’s School of Medicine and University of California, Berkeley. We each bring a background in racial and social justice work and research to our current studies. Our unique dual-degree program affords us the opportunity to build upon these backgrounds, providing instruction and opportunity to question many of the accepted norms of our clinical education.
Dorothy Roberts, a foremost critical race theory scholar (and hero), says in her seminal 2015 TEDMED talk, “Race is not a biological category that naturally produces these health disparities because of genetic difference. Race is a social category that has staggering biological consequences, but because of the impact of social inequality on people’s health.”
In other words, racism, not race, causes health disparities. This truth guides our work. We are united by a common goal: to place justice and challenging anti-Black racism at the center of our practice of medicine to ensure the care and well-being of all communities, especially those that have been historically marginalized and disenfranchised.
As learners of both medicine and critical race theory, we regularly engage in discussions about critical race theory as we study racial disparities in health. We are able to see both at once, in ways that many fellow learners can’t yet see. We also care for underserved patients of color at community clinics and safety net hospitals throughout the Bay Area. These opportunities have allowed us to put theory into practice, and the results are shocking. There are critical, deadly errors in traditional clinical textbooks, research, and practice that contribute to root causes of racial health disparities:
-
In our textbooks, we are taught that race can serve as a risk factor for disease. Yet we know that race is a social construct, not a biological risk factor.
-
In clinical research, we are told that disparities in disease among Black and brown communities are due to culturally determined individual behaviors. Yet we know that structural barriers to food and stress-free lives, as well as targeted discrimination, prevent many people of color from achieving health and well-being.
-
In clinical practice, we are mentored by clinicians who blindly follow guidelines that instruct them to prescribe based on race rather than overall effectiveness. Yet we know that these guidelines are built on a deep history of biological racism and othering within medicine and health care.
We have found these scenarios to be commonplace and largely unchallenged throughout our medical education and training. Racist, outdated notions are taught in clinical education, solidified in research and perpetuated in practice.
We are astounded, outraged, and driven to make a call to action.
This action is personal, political, and technical. We follow the tradition of women of color scholar-activists, like Dorothy Roberts, Cherríe Moraga, Gloria Anzaldúa, and countless others, who embrace that the way we move through the world, our “personal” lives, are inherently political—a “theory in the flesh.” As physicians-in-training, our world is furthermore inherently technical as we learn the algorithms of diagnoses, and those diagnoses are sometimes visibly and sometimes invisibly political. It is all connected. Therefore, this work presented here is unapologetically personal, political, and technical. These are the lives we live and the lens we bring to building a just, antiracist field of medicine.
As physicians-in-training, our world is furthermore inherently technical as we learn the algorithms of diagnoses, and those diagnoses are sometimes visibly and sometimes invisibly political. It is all connected. Therefore, this work presented here is unapologetically personal, political, and technical. These are the lives we live and the lens we bring to building a just, antiracist field of medicine.
Our politics, purpose, and intentions to further advance an antiracist, people-centered medicine are inspired by abolitionist frameworks of those who seek the end-of-the-prison industrial complex. Central to the abolitionist framework is the understanding that all cages that restrict autonomy and expose people to harm—physical, mental, emotional, psychological, and structural—are connected. So, too, in medicine are all the forms of racism connected, and much like abolitionism, in order to fight them, we must see them in their entirety and then work to eradicate them all. The current medical and health-care system in the United States harms Black and brown bodies and souls. To build a medical system in which all people are valued and healed as whole persons, we must challenge the current understanding of what is “normal” and what is “just reality.” We hope that this paper contributes to the abolition of outdated, oppressive “normal ways of doing medicine” that have exploited Black and brown bodies. Ultimately, by deconstructing current limitations, we will collectively generate new imaginations of whole-person healing for communities that have been neglected and ignored. Through this work, we aim to abolish the biomedical oppressions that have put forth more harm than healing in order to reimagine ways to bring healing back to our people.
Central to the abolitionist framework is the understanding that all cages that restrict autonomy and expose people to harm—physical, mental, emotional, psychological, and structural—are connected. So, too, in medicine are all the forms of racism connected, and much like abolitionism, in order to fight them, we must see them in their entirety and then work to eradicate them all. The current medical and health-care system in the United States harms Black and brown bodies and souls. To build a medical system in which all people are valued and healed as whole persons, we must challenge the current understanding of what is “normal” and what is “just reality.” We hope that this paper contributes to the abolition of outdated, oppressive “normal ways of doing medicine” that have exploited Black and brown bodies. Ultimately, by deconstructing current limitations, we will collectively generate new imaginations of whole-person healing for communities that have been neglected and ignored. Through this work, we aim to abolish the biomedical oppressions that have put forth more harm than healing in order to reimagine ways to bring healing back to our people.
We are not the first to make this call. We are led by womxn of color; scholars and activists who have been making this same call for far too long. Yet our experiences as trainees reflect how racism continues to be deeply ingrained in health care. Medicine, and health care more broadly, has yet to heed their call. We have found many practicing clinicians and professors to be unfamiliar with the historical context and harm of their practices. Some are simply ignorant of the impact of their actions. We hope this paper may provide them with the education and language to pause, reflect on their complicity, and begin to question and to shift their practice. Others do not care. We hope this paper begins critical dialogue and change that one day will change their practice as well because we know how deeply historical scars run in medicine.
This is our action. As members of the health-care workforce, we find the current state of racism in medicine untenable. We refuse to be part of a system that perpetuates harmful, deadly practices against Black people and people of color. We aim to use our unique positionality and experiences as medical and graduate students to offer a way forward for our current and future instructors, colleagues, and mentees. We are inspired by the growing body of research and commentary by clinicians and learners challenging both the normalized uses of biological race and the unacknowledged racism in clinical research, education, and practice. Our aim is to amplify existing voices in this movement and to further bridge the gap between critical race theory and medicine.
Our responsibilities to patients, to communities, and to justice demand we make this call to action.
Who Is This Work For?
In thinking about our intended audience for this paper, we are inspired by Michelle Alexander’s preface to The New Jim Crow. ,
,  Our paper is intended for a similarly specific audience—our fellow clinicians in training and current providers of all types, who care about practicing antiracist medicine but who, for a number of reasons, may not yet appreciate the magnitude of the violent history and current clinical manifestations of the flawed assumption about biological race that pervades medicine. We have spoken to countless medical students and current providers who struggle to challenge their teachers and supervisors who perpetuate racist ideologies, due to unfair power dynamics and a lack of readily available facts and data to back up their claims. In part, we have written this resource because we wish it existed for us.
Our paper is intended for a similarly specific audience—our fellow clinicians in training and current providers of all types, who care about practicing antiracist medicine but who, for a number of reasons, may not yet appreciate the magnitude of the violent history and current clinical manifestations of the flawed assumption about biological race that pervades medicine. We have spoken to countless medical students and current providers who struggle to challenge their teachers and supervisors who perpetuate racist ideologies, due to unfair power dynamics and a lack of readily available facts and data to back up their claims. In part, we have written this resource because we wish it existed for us.
We also write this paper for patients. Our desire to support patients in feeling happy, healthy, and strong, rather than pathologized, is why we do this work. However, while we do our best to make both technical medical language and critical race theory accessible for all, we realize that may not be accessible for all our patients. Know that when you say that medicine is hostile, we hear you. We hope for future resources more specifically directed at patients to supplement our work, and more importantly, we hope for medicine to transform into a welcoming practice.
We hope this resource is used as educational and action-generating. Although not exhaustive as an educational resource, we are bridging existing work on critical race theory with our firsthand knowledge of clinical education, research, and practice. Please see the appendix for further resources.
Yet it is not enough to simply read and learn; we must also act. Reflecting on the tenth anniversary of publishing The New Jim Crow, Michelle Alexander notes that this work is necessarily personal, moral, and spiritual. We echo that call and add that it is necessarily political. We live lives that are personal, political, and medical, so our action must be all three as well. We live in a world structured by racism, meaning in order to make the changes necessary to support the health of all communities, we have to continue to unpack the unquestioned uses of race and do the work to reprogram ourselves away from racialized algorithms. We must do the work to build systems that are just and antiracist. Our final section includes our calls to action and a few ideas of where to start. But this is where you must take up your own action so that together we build the health system we wish to live and practice in.
We live lives that are personal, political, and medical, so our action must be all three as well. We live in a world structured by racism, meaning in order to make the changes necessary to support the health of all communities, we have to continue to unpack the unquestioned uses of race and do the work to reprogram ourselves away from racialized algorithms. We must do the work to build systems that are just and antiracist. Our final section includes our calls to action and a few ideas of where to start. But this is where you must take up your own action so that together we build the health system we wish to live and practice in.
Executive Summary
By Noor Chadha, Bernadette Lim, Madeleine Kane, and Brenly Rowland
(Click to download a PDF of the Executive Summary)
 The use of biological race in medicine is an unchallenged, outdated norm throughout clinical education, research, and practice. Medicine largely frames racial health disparities in terms of biological difference and individual behavior, despite evidence that social and structural factors generate and perpetuate most health issues. In particular, racism, a structure and ideology that oppresses and limits resources to minority groups, is rarely discussed in clinical health and the health sciences as a meaningful determinant of health outcomes. Racial health disparities are often wrongly attributed to biology and physiology of racial groups rather than the stratified socioeconomic opportunities that are available. This is bad and irresponsible science.
The use of biological race in medicine is an unchallenged, outdated norm throughout clinical education, research, and practice. Medicine largely frames racial health disparities in terms of biological difference and individual behavior, despite evidence that social and structural factors generate and perpetuate most health issues. In particular, racism, a structure and ideology that oppresses and limits resources to minority groups, is rarely discussed in clinical health and the health sciences as a meaningful determinant of health outcomes. Racial health disparities are often wrongly attributed to biology and physiology of racial groups rather than the stratified socioeconomic opportunities that are available. This is bad and irresponsible science.
“Toward the Abolition of Biological Race in Medicine: Transforming Clinical Education, Research, and Practice” is written by four medical students and graduate student researchers who witness these harms every day in their textbooks, classrooms, clinics, and communities. The paper bridges existing research by critical theory scholar-activists and researchers, and aims to guide clinicians and student learners in medicine, public health, and beyond on why the use of biological race must be abolished in medicine and clinical research, education, and practice. This paper uses an abolitionist framework, fully embracing that anti-racist work in the field of medicine is inherently personal, political, and technical. After establishing that racism, not race, causes health disparities, the paper reveals the violent history of racism in medicine. From this foundation, the paper draws on current examples of the use of biological race in medicine to highlight the urgent need to transform these outdated practices and center patient care.
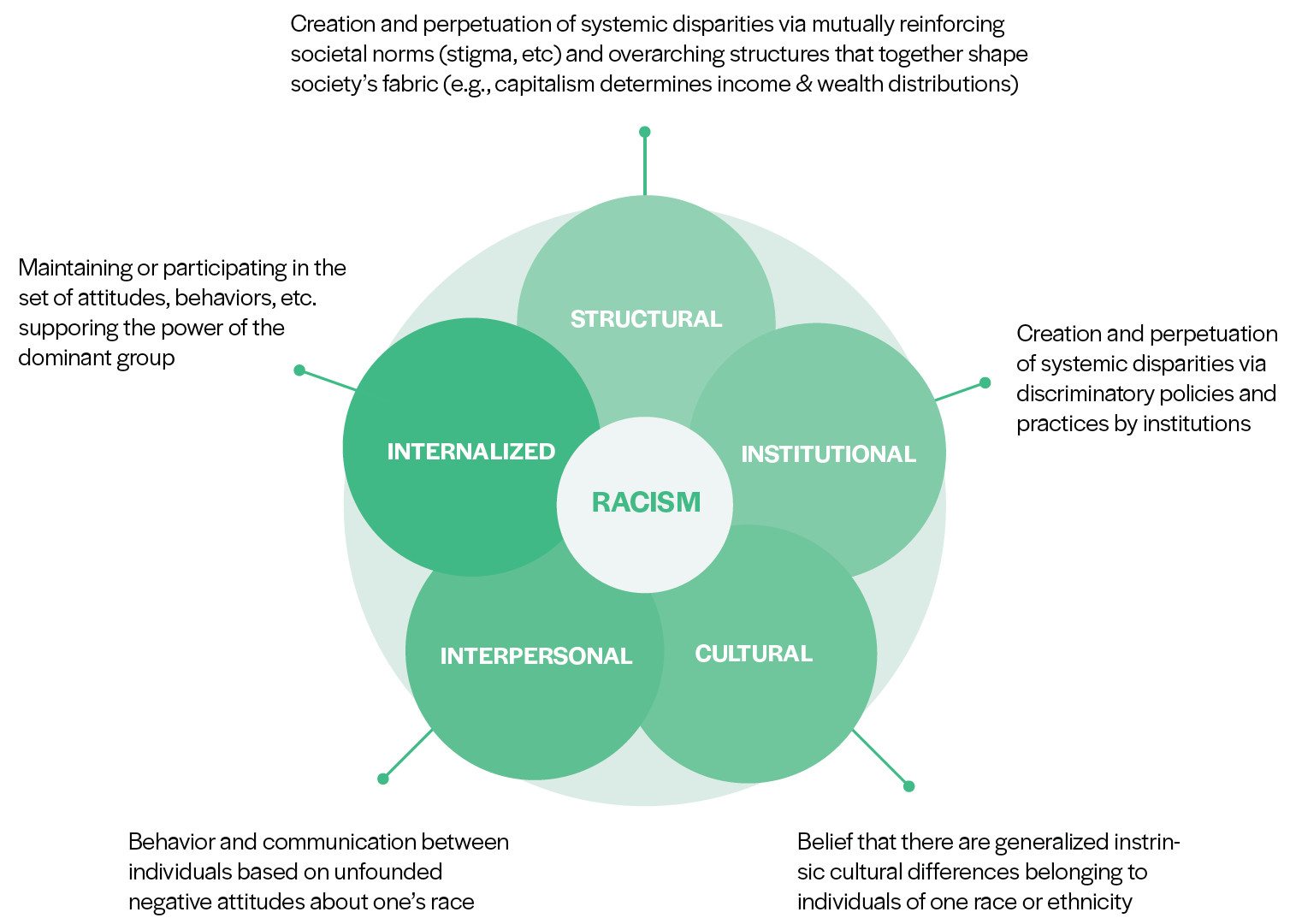
Racism, Not Race, Causes Health Disparities
Racial health inequities exist and persist. In the United States, this can be seen by the disparately higher rates of cardiovascular disease, renal disease, diabetes, strokes, certain cancers, low birth weight, preterm delivery, and other health problems among people of color (often Black people) compared to white people. Biomedicine tends to interpret these disparities as evidence of fundamental genetic differences between socially constructed racial categories. Yet, long-standing advocacy by scholars and activists of color and a growing body of evidence from medical journals emphasize that these health disparities stem from inequalities in power and socioeconomics, not from genetics. Racism functions on several different levels (internalized, interpersonal, cultural, institutional, and structural) and drives these social and structural determinants of health disparities.
Cranial Capacities to Eugenics: How Medicine and Health Sciences Biologized Race
The conceptualization of race as biology is rooted in colonization. Scientific racism emerged from theories of biological inferiority, including Carl Linnaeus’s polygenism and Dr. Samuel Morton’s efforts to compare cranial capacities of white colonizers, native people, and enslaved people. These flawed theories cemented societal conceptions of skin tone differences and non-whiteness as biological concepts. Such historical context laid the groundwork for racial inequality, including the expropriation of property from natives, denial of political rights, slavery and other forms of coercive labor, and explicit extermination and lynching of non-white people.
A clear thread can be drawn from the scientific racism of scientists like Linnaeus and Morton in the nineteenth century to institutionalized racism in science and medicine today. Morton was a part of the “American School” that perpetuated social Darwinism, a theory claiming that certain groups of people were “less fit” than others, and therefore less deserving of survival. As these worldviews began to popularize and become normalized in scientific and everyday discourse, it paved the way for the eugenics movement of the twentieth century. Eugenicists repeated the arguments of social Darwinists before them. In both Europe and the United States, eugenicists aimed to encourage the reproduction of more “fit” races and extermination of those who were “biologically inferior.” In the United States, eugenics took the form of forced sterilization, segregation, and antimiscegenation laws, all specifically aimed at the extermination of nonwhite people. In Germany, Nazi doctors practiced eugenics by slaughtering, torturing, experimenting on, and murdering millions of people. The perpetrators of these crimes were trained physicians and often distinguished scientists who were inspired and actively influenced by eugenicists in the United States. This legacy underlies the practice of race-based medicine today.
Race-Based Medicine in Diagnosis and Treatment
The current misuse of race as a risk factor is rampant across clinician discussions including but not limited to hypertension, kidney disease, lung function, and genetics. This misuse is harmful and violent to patient care of Black and Brown communities. Clinicians often use a patient’s skin color, race, and/or ethnicity as heuristics to determine their diagnosis and treatment plan. In fact, race serves as a shortcut for clinical thinking from the onset of medical training. This shortcut can be dangerous and inaccurate. Firstly, it enforces racial bias that may be present or introduces new ones. This translates directly to clinical care, where a patient’s race is seen as a risk factor for disease and requires that providers associate certain illnesses with certain races. As such, providers may overlook diseases in patients of races and ethnicities that are not traditionally associated as “risk factors.” They may also never inquire into the root causes of illness for a person experiencing racism and inequality (such as structural and social determinants of health) or may miss more complicated and nuanced diagnoses. Furthermore, race is dangerously built into algorithms that are standardly used for diagnosis across various fields of medicine, especially for cardiovascular disease, kidney disease, lung function, and genetics. This paper details more carefully how these faulty algorithms are embedded in everyday medicine, noting how what could be considered “normal” function for Black people is repeatedly considered pathologic or unhealthy for white people. This discrepancy leads to late diagnoses and poorer treatment for Black people compared to their white counterparts.
Looking Ahead: Epigenetics
Despite the many ways in which new scientific developments like precision medicine threaten to entrench biological racism, new fields such as epigenetics, developmental origins, and life course research are contributing to our understanding of how racism, not race, has biological effects on the body. In this section, we talk more about how epigenetics and other biopsychosocial fields are pulling together biology, psychology, and upstream determinants of health to answer how racism “gets under the skin.” We show how the social and structural determinants of health (mediated or created by racism) can literally embed themselves in our cells and result in the health disparities and injustices we witness today.
Visions forward:
As physicians-in-training, we envision a world where the social construct of race is not conflated with biology, and where the health consequences of racism are acknowledged, addressed, and cared for in all their forms.
To make this a reality, medicine must adopt antiracist institutional practices regarding research, practice, and education.
- Medicine must unveil and teach how racism has shaped scientific advancements, tools, and diagnoses.
- In order to account for the health consequences of racism, clinicians should prioritize social history intake and be aware of how social and structural stressors perpetuate racial health inequities.
- We must adopt the same standards and guidelines for diagnosis and treatment of all patients regardless of race.
- Race cannot and should not be used as a biological determinant in clinical guidelines nor the research informing them. Rather, clinical guidelines on racial health outcomes must take into account the consequences of racism in racial health disparities. Racial differences are not the cause of disparities; they are the result of multilevel racism.
- Health-care providers play a key role in combating racism. In order to support their patients in feeling happy, healthy, and strong, clinicians must seek to affirm the strengths their patients bring, not assume they are a collection of risk factors. Clinicians need a paradigm shift to approaching patients of color as whole, rather than broken.
- Medicine must break down its own intellectual silos and hierarchy to build interdisciplinary alliances with thought leaders who have built foundations on the intersections of racism and health. Rather than using race as a differential diagnosis shortcut, elimination of race-based medicine presents an opportunity to call for interdisciplinary dialogue and action in solidarity with those from affected communities, critical race theorists, community-based organizations, and racial justice initiatives.
Introduction
Toward the Abolition of Biological Race in Medicine: Transforming Clinical Education, Research, and Practice, written by the Abolishing Biological Race in Medicine Working Group of the Freedom School for Intersectional Medicine and Health Justice, bridges existing research by critical theory scholar-activists and researchers to guide clinicians and student learners in medicine, public health, and beyond on why the use of biological race must be abolished in medicine and clinical research, education, and practice. We begin with how medicine is rooted in a violent history of racism and has scientifically codified race as a biological construct throughout history. From this foundation, we draw on current examples of the use of biological race in medicine to highlight the urgent need to transform these outdated practices and center patient care. Throughout the paper, we intersperse quotes and anecdotes that have been shared with us by our medical student peers.7
Our paper includes four main sections:
- Section 1: Racism, Not Race, Causes Health Disparities
- Section 2: Cranial Capacities to Eugenics: How Medicine and Health Sciences Biologized Race
- Section 3: Race-Based Medicine in Diagnosis and Treatment
Drawing on existing research examples of heart disease, hypertension, BiDil, kidney disease and glomerular filtration rate, lung function and spirometry, and genetic ancestry or precision medicine, we argue that current use of race is not only outdated but harmful and violent to patient care of Black and brown communities.
- Section 4: Looking Ahead
These are our key takeaways:
- Medicine has willfully ignored its racist history despite ongoing calls from scholars and activists to rectify its violent and oppressive history. This has resulted in medicine continuing to inflict and perpetuate racism that harms communities of color.
- Using biological race as a heuristic for diagnosis of disease and interpretation of symptoms masks racism.
- Because of the biological use of race in clinical guidelines and education, patients of color are being systematically misdiagnosed and undertreated and are at risk for bad health outcomes.
- Race-based medicine teaches people of color that their bodies and communities are abnormal, deficient, and broken, increasing stress and the burden of racist stigma. Medicine is an unwelcoming, hostile space for people of color.
- If we don’t dismantle race-based medicine, it will be perpetuated, ultimately harming patients in real, concrete ways.
As physicians-in-training, we envision a world where the social construct of race is not conflated with biology and where the health consequences of racism are acknowledged, addressed, and cared for in all their forms.
To make this a reality, medicine must adopt antiracist institutional practices regarding research, practice, and education.
Section 1: Racism, Not Race, Causes Health Disparities
What Are Racial Health Disparities and Why Do They Exist?
Racial health inequities exist and persist. According to the Kaiser Family Foundation, racial health disparities are the “higher burden of illness, injury, disability, or mortality experienced by one (politically and socially constructed) population group relative to another.”8 We use racial health disparities synonymously with racial health inequities, although we acknowledge there are subtle differences and that inequities is preferred by some because it draws attention to the power imbalance at the root of the issue.9
In the United States, this can be seen by the disparately high rates of cardiovascular disease, renal disease, diabetes, stroke, certain cancers, low birth weight, preterm delivery, and more between people of color (often Black) and white people.10 Biomedicine tends to interpret these disparities as evidence of fundamental genetic differences between socially constructed race categories. Yet, a growing body of evidence from medical journals emphasizes that these health disparities stem from inequalities in power and socioeconomics, not from genetics (for more on the body of evidence, see appendix 1).
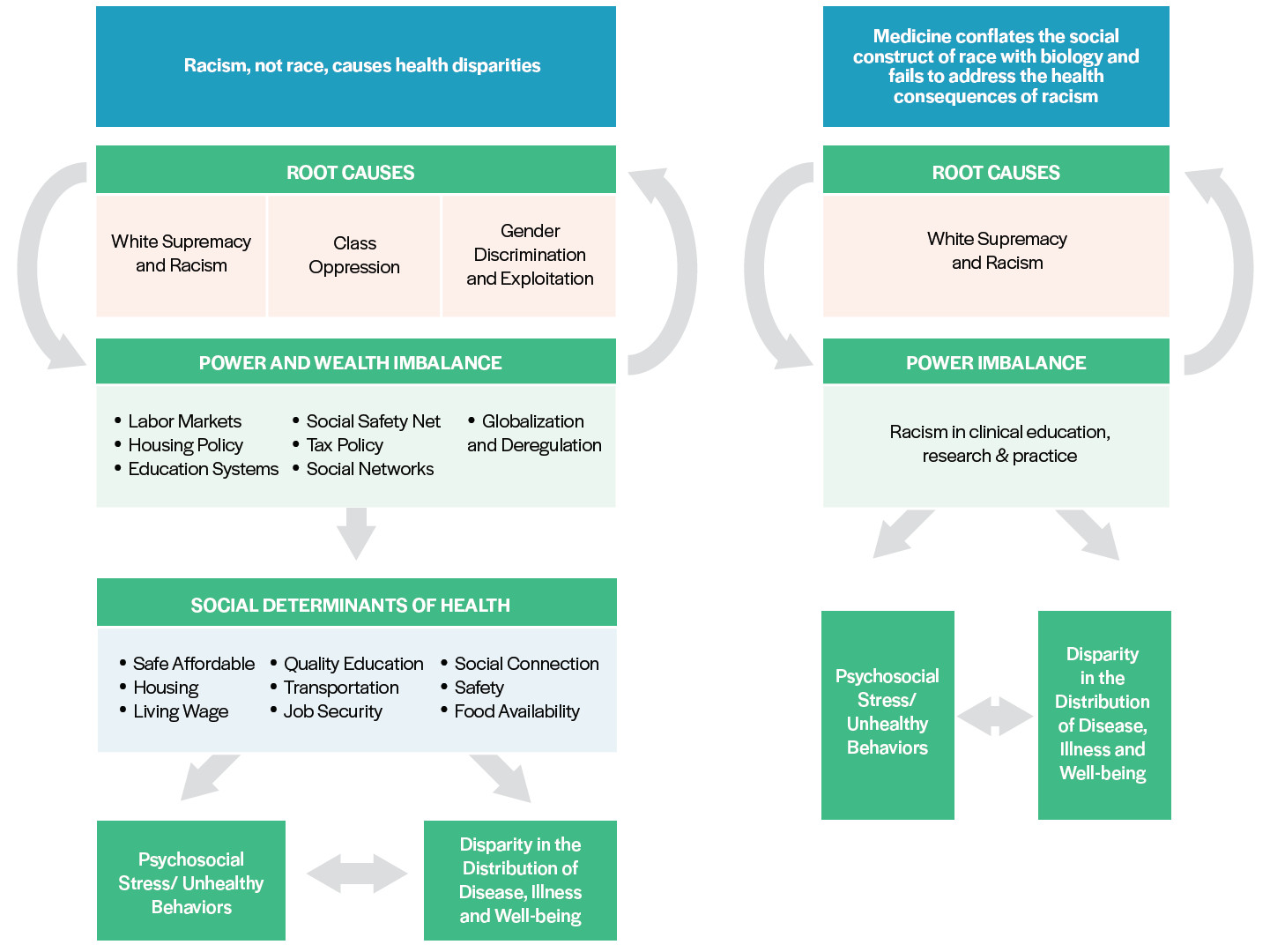
Dr. Joia Crear-Perry, a fierce physician advocate for Black maternal health equity, adapted the guiding mantra that “racism, not race, causes health disparities,” as seen in the following graphic to show the mechanisms of how racism causes health disparities.11 We adapted her model (on the left) to show how this works in clinical education regarding the use of “race as biology” (on the right). In this section, we explain how racism causes health disparities, our model, and how we define the terms we are using. Rather than use heuristics and simplifications, it is critical that we as a medical profession address racism head on and in all its subtleties.
Source: Graphic adapted by Dr. Joia Crear-Perry, originally from Tackling Health Inequities through Public Health Practice, by R. Hofrichter and R. Rhatia.
Dr. Crear-Perry shows that health disparities start with root causes (racism and white supremacy, class oppression, gender discrimination, and exploitation) to create deep power and wealth imbalances across much of the systems that govern our lives, such globalization and deregulation, labor markets, housing policy, education systems, and much more.12 These, in turn, mold the social determinants of health by shaping who is paid how much and with what benefits or job security, who is allowed to live where, what quality of housing they can afford, what quality of education exists for them or their children, what quality of food is available, and much more. These mean that differential power distributes the social and environmental determinants of health differently, depending on who holds and doesn’t hold power. In the United States, this tends to fall primarily along race, class, and gender lines, with those who hold multiple marginalized identities, such as Black working-class women, even further marginalized. These social determinants of health lead both to an unequal distribution of disease and well-being (e.g., increased asthma rates in neighborhoods with poor quality housing and increased environmental exposures) as well as psychosocial stressors and unhealthy behaviors.
For our focus as medical students, when clinical education and medicine at large conflate the social construct of race with biology, it entrenches racism across the system. This means we as providers not only fail to address in practice how racism is creating health disparities, we also create and perpetuate racial health disparities. We define institutional and structural racism in this paper, but a system that is racist produces power imbalances along race in medicine, leading to racism in clinical education, research, and practice. We argue that this racism encourages providers and researchers to largely ignore social determinants of health, and instead focus on the most individual and most superficial aspects of health inequities—skin color as a predictor of epidemiological “risk,” individual behavior, etc.
Many health-care practitioners and researchers—even those who pursue justice and equity through their work—will ascribe observed racial health disparities to essentialized notions of biological racial difference. A recent study shows an alarming number of medical trainees wrongly believe Black people literally have thicker skin that biologically accounts for a perceived higher pain tolerance.13 This and several other examples outlined in this paper (such as the calculations for kidney function) show how physicians conflate racial health disparities with biological difference, affecting how physicians diagnose and treat patients of color and directly causing a differential distribution of certain diseases by race. This conflation asserts a (false) naturalized racial hierarchy and perpetuates flawed science. Furthermore, it fundamentally distracts from the true ills that negatively impact people’s health outcomes and well-being: racism as a root cause of inequities in society.
Many more health-care practitioners do not question the rubrics in the differential diagnoses that assign individual “risk” for different diseases or illnesses based on only epidemiological population data or assumptions on individual behavior based on skin color or culture. These assumptions obscure the power differences that shape social determinants of health, which is why our diagram skips the social determinants entirely, because we are taught to gloss over or blatantly ignore them in our training, instead exhorting our patients to simply “eat better and walk more.”
All of these add up. This confusion and unquestioned acceptance of biologization of race in differential diagnoses and medical education has dangerous consequences: patients who are diagnosed later and with worse outcomes, given health education that doesn’t address their lived experience, and whose care directly causes psychosocial stressors based on their perceived race.
This inattention to root cause and direct creation of health inequities is our call to action. Through this paper, we hope clinicians, researchers, educators, and students will join us in our vision of a world where the social construct of race is not conflated with biology, and where the health consequences of racism are acknowledged, addressed, and cared for in all forms. To understand this graphic better, we further define racial health inequities, race, white supremacy, and the five types of racism, key terms that are the foundation of our vision.
In order to understand how medicine can become antiracist, we must first be on the same page about what racism truly is and how it harms our communities. Therefore, in order to highlight the intentionality underlying the language we use throughout the rest of our paper, we will next define key terms relating to race and racism.
A Note about Language
Throughout this paper, we strive to follow the example of critical race scholars and activists before us in the language we use. Critical race theory states that race is constructed by society and places the construction of race and the resulting racism at the center of any analysis. These scholars include W.E.B. Du Bois and Kimberley Crenshaw, whose work has taught us to capitalize the word “Black” when referring to Black people. Crenshaw states, “I capitalize ‘Black’ because ‘Blacks, like Asians, Latinos, and other “minorities,”’ constitute a specific cultural group and, as such, require denotation as a proper noun. By the same token, I do not capitalize ‘white,’ which is not a proper noun, since whites do not constitute a specific cultural group.”14 Although we acknowledge that the concept of “white” as a cultural group has been since questioned, we follow this notation except when directly quoting from other sources.
Race
Defining the roots of race has been and continues to be a point of contention. Despite different perspectives, race and racism have pervaded the social and political fabric of the world. Particularly in the United States, racism is at the epicenter of inequalities in income, health, and life outcomes.
Race is a social category constructed by socioeconomic and political forces that determine its content and importance.15 In other words, race is determined by how society perceives you and you perceive society, which in the United States is largely centered around skin color and other arbitrary markers of difference from “whiteness.”16 Race exists as a sociopolitical category with origins in oppression. Race has no biological basis.
Biomedical researchers and social scientists have established that the concept of race cannot adequately or accurately describe global human genetic diversity.17 Populations cannot be distinguished by clear sets of genetic markers, and there is vast genetic variation within each so-called race, with more diversity within populations than between populations. There is vast genetic variation across the entire human species, and relatively little genetic variation between racially defined groups. The traits falsely used to distinguish races do not predict other biological traits.18
In medicine and health research, race must be distinguished from ancestry, which refers to a person’s genealogical history.19 The concept of race is an inadequate proxy for the genetic and cultural variations that can result from differing ancestral origins due to the arbitrary categorization of cultures and people under “race.”20 The conflation of race with ancestry perpetuates false science and can unintentionally perpetuate racism in biomedicine.21 Any discussion of ancestry and race in clinical medicine must also acknowledge that ancestry and genetics are just one small piece of the puzzle, which should include the social and structural determinants of health discussed previously. For more on the difference and its use in medicine and research, see Section 3: Race-based Medicine in Diagnosis and Treatment.
Race has no genetic or scientific basis. While there are certainly population differences between groups from around the world, the biological signatures that make up a population do not align with social categories or understandings of race. Throughout this paper, biological racial difference will be used to call out the false idea that there is a natural, biological difference between individuals who identify according to politically and socially constructed categories of race.
It is critical to our vision that medicine disentangles itself from these false ideas of biological difference based on race.
White Supremacy
The construct of race provides the foundation for white supremacy, which is both a political ideology and a racist belief that is woven throughout the foundation of the health systems in the United States. It endorses the superiority of the white race both overtly and in less visible ways. White supremacy maintains and endorses the societal structures wherein white people hold the most power. This can be traced from the beginning of the United States to present day and does not necessarily function in a linear or singular way. Scholar Andrea Smith provides one framework for understanding the mechanisms of white supremacy, wherein it is upheld by three distinct but interrelated logics.22
Logic 1: Slavery and Capitalism
The logic (or logical foundation) of slavery values Blackness as nothing more than property and potential profit. Capitalism demands that a laborer’s work becomes a commodity, and those at the bottom of the hierarchy must offer up even their embodied selves as a potential for profit for someone else. This hierarchy is maintained by the logic of slavery. Thus, at the root of anti-Black racism, Black folks’ humanity is denied and valued only by their production capability and exploitative profit. This logic continues in modern day, most notably reflected in the current carceral system.
Logic 2: Genocide and Colonialism
In order for non-Indigenous people to claim ownership and governance over the United States (colonialism), Indigenous people must disappear (genocide). This is enacted both physically—from the historical murder, removal, and segregation of Native Americans to the current systematic disinvestment and breaking of treaties—and with cultural norms that erase Native American peoples and their sovereignty from the collective dominant psyche. This logic was most recently disrupted in recent protests at Mauna Kea and the Dakota Access Pipeline.23 24
Logic 3: Orientalism and War
Throughout history, the West (both the United States and broader colonial powers) defined itself in opposition to the “exotic” and inferior “Orient” (defined more broadly than just Asia). These people thus are defined as inferior and posing a constant foreign threat to the “empire.” This constant implication of war leads to xenophobia and anti-brown racism against Asian Americans, Arabs, Hispanics, and more, justified by the need for strength against the “invading threat.”
These logics are interlocking and reinforcing, but all ultimately ensure that whiteness is privileged and kept in power above all others. White supremacy is at the root of all types of racism outlined below and thus at the core of racist health-care practices and health disparities. We see this in the clinical guidelines and medical texts discussed throughout this paper. White supremacy creates a racial hierarchy throughout the structures of our world and is at the root of the conflation between race and biology in order to establish the “(false) naturalized racial hierarchy” mentioned previously. A key fundamental result in medicine of white supremacy is that people of color are inherently viewed as carriers of disease.
While this paper is designed to be educational, it is by no means exhaustive. We hope that those who are ready to eradicate the harms of the legacy of racism in the field of medicine continue to read both our work and the cited sources, many of which are authored by Black and Indigenous scholars of color who have done tremendous work to bring these conversations to the world (see appendix for further reading).25
Racism
Racism is a system of power that upholds the political and social capital of white supremacy in the United States. Racism is deeply embedded in social, political, and economic structures. Most popular perceptions of racism only address the interpersonal prejudice, discrimination, or antagonism based on the belief that certain racial groups are superior to the other. But this only addresses one small part of the ways that racism is embedded in people’s assumptions, institutions, and structures. Thus, racial prejudice, as just one aspect of racism, refers specifically to discriminatory attitudes and actions between people based on the assumption that a particular race is superior or inferior to another, and that a person’s race defines a person’s internal traits.26 Power refers to authority granted by sociopolitical and economic structures for access to sources, to reinforce racial prejudice.
Racism produces and reproduces social, economic, and political inequalities, and is thus a fundamental cause of disease. Racism is complex and interwoven, and beginning to be studied as a determinant of health and outcomes. But these studies have not been sufficiently incorporated into medical and clinical education, research, and practice.
In order to address the many ways racism can shape medicine, we categorize it into internal, interpersonal, cultural, institutional, and structural levels. These levels interact with and work upon each other to reinforce racial hierarchies and can be experienced simultaneously.
Together, these levels make up the society in which we practice.
Although many other disciplines use “systemic racism” to describe the entrenched racially prejudiced power differentials mediated by institutions, we use “structural racism,” as this is the nomenclature we have been taught in public health and medicine. We agree with the Aspen Institute that structural racism tends to include an analysis of the “historical, cultural, and social psychological aspects of our current racialized society,” which we strive to include in our work here.27 However, for the purposes of interdisciplinary dialogue and learning, we propose they are similar enough to be considered synonyms.28
The following examples demonstrate how racism functions on various levels to create, perpetuate, or exacerbate health disparities, although it is nowhere near exhaustive.
Interpersonal Racism
Definition: Interpersonal racism is behavior and communication between individuals based on unfounded negative attitudes about one’s race or culture. There is a wide spectrum of interactions that can occur under the category of interpersonal racism from explicit direct violence to “implicit” microaggressions, all of which have negative consequences on health outcomes.
Interpersonal racism is often understood as the “classic example” of racism—the harassment and violence associated with the civil rights movement, Jim Crow, and other points in history. It’s important to acknowledge that although strides have been made, interpersonal racism includes all-too-common microaggressions and that interpersonal racism is just one of many interlocking forms of racism that medicine must address.
In medicine, interpersonal racism affects both providers and patients of color. One current issue is the racial microaggressions in the clinical learning and care environment, which have consequences beyond the “micro,” such that these negative interactions falter trust between patients of color and health-care providers.29 Defined as “the everyday verbal, nonverbal, and environmental slights, snubs, or insults, whether intentional or unintentional,” microaggressions can be found in everyday conversations and encountered in any social setting.30 These range from being assumed to be a criminal, being presumed to be inferior, being exoticized, or being treated as a second-class citizen. Examples of microaggressions in a clinical learning environment include telling high-achieving students of racial or ethnic backgrounds that they are “smart for a [insert ethnicity] person,” expecting an individual of any particular group to “represent” the perspectives of others of their race, and singling individuals out because of their backgrounds. These can alienate learners, exacerbating imposter syndrome and dropout rates, as well as directly affecting health.31
Direct health consequences of microaggressions include greater perceived stress, depressive symptoms and negative affect, and physical health issues such as increased history of heart attack, pain, and fatigue.32 These experiences of discrimination for trainees and patients have been associated with elevated blood pressure, breast cancer, low birth weight, lower back pain, and more.33
Finally, while microaggressions can be perceived as harmless, such racial stereotypes can ultimately become matters of life or death. The deaths of Trayvon Martin and Michael Brown are a result of interpersonal racism colliding with structural factors: the negative racial stereotypes assuming Black boys are criminals alongside policies that allow for and encourage unnecessary lethal force results in continued tragic killings and the ongoing threat of violence to the community.34
In the field of medicine, attempts to address interpersonal racism have focused almost exclusively on implicit bias. Implicit bias is a psychological concept that embedded stereotypes affect decision-making without conscious thought, which is often interpreted as an individual problem when in fact it stems from and resonates with structural oppression. In health care, this leads to poor interpersonal and systemic outcomes, such as lower empathy, higher distrust, and lower referral rates for specialty care.35 Yet most trainings do not grapple with racism in its entirety and let providers “off the hook” for owning and addressing the effects of racism in health care. Implicit bias work doesn’t usually address the structural and systemic forcible exclusion or pathologization of brown and Black bodies. Many implicit bias trainings get hung up on “intention” and the assumption that these biases are unintentional, which allows providers to continue to think of themselves as fundamentally good people. But the narrow focus misses the multitude of ways racism functions in medicine and doesn’t create a way for health-care providers to see and address our complicity in these systemic harms (which function whether or not we have good intentions as individuals). Furthermore, rather than a paradigmatic shift like that of cultural humility (over its predecessor, cultural competency), implicit bias is often seen as yet another training, a knowledge to be acquired in isolation from the historical and multifaceted context of racism.
Rather than a reliance on individual knowledge, we encourage the practice of self-interrogation of potential micro- and macroaggressions in the medical field. This not only will encourage ongoing reflection but likely will require providers to acknowledge and address more systemic and structural factors.
Internalized Racism
Definition: Internalized racism occurs when “a racial group oppressed by racism supports the supremacy and dominance of the dominating group by maintaining or participating in the set of attitudes, behaviors, social structures, and ideologies that undergird the dominating group’s power.”36 Internalized racism is a product of internalized colonialism, in which nonwhite colonized people begin to uphold the values and social signifiers of white colonizers and lose identities.
Internalized racism has significant mental and physical health consequences, including negative self-esteem, a sense of inferiority or victimhood, ethnic self-hatred or self-doubt, and navigating the additional emotional burden of overcoming racialized or stereotype-driven interactions.37 In addition, internalized racism contributes to the perpetuation of negative racial stereotypes not only by dominant cultures (e.g., white people), but also within racial groups themselves.38
With regards to physical health, a long-standing and widespread social phenomenon that is a consequence of internalized racism can be seen in the practice of skin whitening among immigrants from, and individuals living in, formerly colonized places such as the Philippines, India, and Nigeria.39 Finally, emerging research suggests that internalized racism has effects on body mass distribution and insulin resistance.40
Potential remediation of internalized racism includes increasing awareness; reframing racism away from the individual (adopting a systemic and structural understanding aimed at liberation from oppression); increased training for providers, researchers, journalists, and others to recognize internalized racism as well as stop perpetuating potentially harmful interactions; and providing opportunities for in-group healing dialogues.41 The field of medicine can begin to address internalized racism by increasing awareness across providers, affirming patients’ strengths and humanity, and incorporating antiracist policies and practices across systems.
Cultural Racism
Definition: Cultural racism occurs through belief that there are generalized intrinsic cultural differences belonging to individuals of one race or ethnicity. It is important to note that race and ethnicity are social categories. While individuals within racial and ethnic groups may have similarities, cultural racism arises in the assumption that everyone in one racial or ethnic group has the same cultural values, habits, and beliefs.
Medicine has a history of aligning cultural generalizations and “behaviors” with risk factors of disease, which perpetuates cultural racism. This practice has shaped clinical practice and research on health disparities by reducing complicated phenomena to broad and oversimplified assumptions of characteristics and behaviors.
Contemporary research in health disparities oftentimes provides the “scientific” basis for clinical overgeneralizations by framing racial groups in ways that perpetuate cultural racism. Perhaps the most overused heuristic is that of diet and nutrition: certain racial and cultural groups are generally assumed to subscribe to a poor diet by “cultural preference” and thus prone to higher rates of certain diseases like diabetes and hypertension.42 Focusing on cultural aspects and individual behavior as sole determinants of racial health disparities is misleading, ignores structural factors that perpetuate disease, and tends to perpetuate notions of racial inferiority and negative stereotyping.
Research also feeds into clinical practice. The 1992 University of California, San Francisco, (UCSF) Nursing Cultural Competency manual organized subsections on common characteristics, habits, and beliefs by race and culture. Mexican patients were characterized as oftentimes “dirty,” having “cultural values that do not believe in regular daily cleansing.” A 1996 publication, Culture and nursing care: A pocket guide, divides care into chapters such as “Gypsies,” “Haitians,” “Japanese Americans,” “Black African Americans,” “South Asians,” and more.43 A presumably “updated” yet similarly divided book published by UCSF Nursing Press by the same authors (Lipson and Dibble) in 2005 states, “Haitians tend to avoid eye contact, are not concerned about sharing personal space with others, and exhibit low threshold of pain.”44 Despite its intent to provide tailored care to diverse patients, cultural competency ultimately operates by relying on assumptions that overgeneralize specific cultural values to all people of a certain race or ethnicity.45 The stereotypes and coarse categorizations of cultural competence in the UCSF Nursing Press books above continue to be cited in more current and progressive-seeming nursing texts, such as Community/Public Health Nursing Practice and Public Health Nursing: Population-Centered Health Care in the Community.46 Cultural competency, still taught and practiced in many institutions today, can thus be seen as a form of cultural racism.
Rather than perpetuating cultural racism and cultural competency in education, research, and practice, new movements in incorporating cultural humility in health-care settings have allowed for self-reflection and lifelong learning.47 Rather than notions of achieving complete “knowledge” and “awareness” of knowing certain cultures, cultural humility centers push for a critical lens to power dynamics as well as learning with and from clients about the cultural values and beliefs they uniquely hold as individuals.
Institutional Racism
Definition: State and nonstate institutions, such as government, education, and health care, create and perpetuate “racially adverse discriminatory policies and practices” disparities in social and structural determinants of health by controlling where people of color can live, learn, work, and play.48 , 49
Medical institutions have both participated in segregation and actively inflicted race-based harm on communities. Two of the most stark examples are the forced sterilization and obstetrics experimentation on womxn of color. From the earliest times of slavery to present day, American society has overtly and subtly tried to control the reproductive capacity of Black women. This has ranged from overt (e.g., forced sterilization, experimentation of new OB-GYN surgeries on slave women, testing the invention of birth control) to more subtle ways (e.g., characterization of Black mothers as both “incurably immoral” and “hyperfertile”).50
Today, Black women are three to four times more likely to experience a pregnancy-related death than white women.51 This maternal mortality crisis is rooted in institutional and structural racism both within and external to the health-care system.
Several medical organizations have issued policy statements about racism and its effects on health. For example, in 2018, the Society for Adolescent Health and Medicine (SAHM) issued a policy paper titled “Racism and Its Harmful Effects on Nondominant Racial–Ethnic Youth and Youth-Serving Providers: A Call to Action for Organizational Change.” The recommendations issued by these, and other, medical organizations are vital steps toward antiracism in medicine. As the SAHM paper states, “Organizations involved in clinical care delivery and health professions training and education must recognize the deleterious effects of racism on health and well-being, take strong positions against discriminatory policies, practices, and events, and take action to promote safe and affirming environments.”52
Furthermore, medical institutions must eradicate the racism currently embedded in everyday clinical guidelines and practice such as those that lead to the current maternal mortality crisis. Institutional policies that disproportionately push women of color to have unnecessary C-sections at far higher rates than their white peers, reduce access to prenatal and postnatal care, and lead to higher rates of untreated chronic conditions are examples of institutional racism leading to disturbing disparities in maternal mortality.
Structural Racism
Definition: Zinzi Bailey et al. (2017) define the difference between institutional and structural racism as follows: “Structural racism refers to ‘the totality of ways in which societies foster [racial] discrimination, via mutually reinforcing [inequitable] systems…(e.g., in housing, education, employment, earnings, benefits, credit, media, health care, criminal justice, etc) that in turn reinforce discriminatory beliefs, values, and distribution of resources,’ reflected in history, culture, and interconnected institutions” (emphasis added).54
These interlocking systems interact to create societal norms or beliefs and create the institutional policies and laws that lead to institutional determinants of health. These overarching structures are called structural determinants of health. Structural determinants of health, including structural racism, build the many facets of the unequal social and physical environment in which we live. Structural racism could therefore be called a “fundamental cause” of health disparities.55 The interlocking systems explain the unrelenting and unequal impact of past policies and laws, which have entrenched inequities by entrenching unequal access across many systems, and continue to reverberate in today’s policies, practices, and laws (today’s institutional racism). To address health disparities without addressing fundamental causes like structural racism is incomplete and inaccurate, and much of the science we critique in this paper lacks that view.
As Bailey et al. note, structural racism begins with the categorization of Black, brown, and Indigenous bodies, creating systems of oppression that are both explicit and hidden from view, as well as propagating violence, even genocide. In today’s world, structural racism affects where someone can live, through past restrictive housing laws and loan availability, whether or not they will be arrested and jailed for minor drug offenses, through the War on Drugs, and many other systems. The interlocking effect has been an “entrenchment of racial economic inequities” as well as exclusion from resources and institutions that promote health and well-being.56 Structural racism ensures that cost, access (financial, geographical, material), language, community influence, and stigma can limit and negatively affect one’s ability to freely access these institutions.
One example of the interlocking systems of structural racism is the exclusion of Black people from housing and employment. After Jim Crow segregation ended, Black people were excluded from the Social Security Act by excluding agricultural and domestic workers (at the time, jobs largely held by Black people) and excluded from the benefits of policies like the GI Bill by de facto exclusion from housing. At the colleges that would accept returning Black war veterans, there was no nearby housing that would be sold to Black people due to practices such as redlining, which structured who could get mortgages after the Great Depression based on the “desirability” of neighborhoods. That desirability score included an assessment of how many Black, immigrant, and other “undesirable” people lived there. Although redlining is no longer legal, its effects continue. One recent study shows that asthma rates continue to be higher in formerly redlined neighborhoods than their surrounding neighborhoods.57 Black families were systematically excluded from wealth creation.
Furthermore, the criminal justice system interlocks with housing and employment to continue the lack of access to housing and employment. The War on Drugs and “tough on crime” policies increased the visibility of this intersection and continue to disproportionately affect Black and brown communities, both through disproportionate incarceration (for the same crimes as white people) and the social, economic, and psychological consequences of incarcerating so many Black and brown people. These interlocking systems continue to affect the health and well-being of individuals and communities through direct and indirect health effects. Bailey et al. report increased levels of myocardial infarctions, low birth weight pregnancies, and psychological stress, both chronic and acute, among many other adverse outcomes.58
These zoning laws and their consequences also create environmental racism, in which predominantly Indigenous, Black, and Latinx people are zoned into areas with environmental hazards ranging from damaging air pollution, to Superfund sites near their homes, to disproportionate burdens of climate changes. These communities are thus overexposed to environmental hazards and bear a disproportionate burden of respiratory and skin diseases, as well as increased epigenetic changes that can later affect their health.59
As medical students, we believe it is crucial to our understanding of the health and well-being of our patients and ourselves, of our society, to know these levels of racism. We must know how they work, how they have worked, and how they will continue to work. Research has begun to scratch the surface of the many ways this plays out in patients’ and providers’ lives, but we must reshape the way we understand and practice medicine and health to include a frank look at the history of the United States’ treatment of Black and brown people, and its consequences for today.
In a society where race has been a normalized part of everyday life, medicine must acknowledge that use of race as a risk factor or predictor of health outcomes is simply false science. Because of its significance in shaping political discourse and social relations in the United States, race has become a social construct and political identity. An individual’s racial identification has real economic and psychosocial consequences on lives, becoming a central influence in US history resulting in unequal outcomes across various life outcome indicators, including income, wealth, health, birth and mortality, and more.
As such, racism, not race, is a key determinant of health. Racism—the discrimination according to one’s racial category—has become an arbiter of health disparities and dismal life outcomes in the United States.
Thus, medicine must come to terms with the two truths:
-
Race has no biological basis.
-
Racism has been and continues to be a key determinant of disparate health outcomes, especially in the United States.
Once we acknowledge the role of all the levels of racism, we can build a better way. Clinics must continue to advocate for policies and laws that address both structural and institutional racism. Researchers must take structural racism into account, no matter their field of study, and begin to study the effects of racism directly. Educators must teach this legacy, and clinicians must know how it affects their patients and their peers. We have to broaden the conversation in medicine and health to include institutional and structural racism alongside the other types in order to create a truly antiracist, just, and healing medical system.
Section 2: Cranial Capacities to Eugenics: How Medicine and Health Sciences Biologize Race
During my first semester of medical school at the Joint Medical Program [JMP], Professor Osagie Obasogie asked another student and me to colead a discussion designed to provide the historical and conceptual context for modern research ethics. Upon doing the readings assigned for the discussion, [we] were shocked and angered that neither of us knew about the history of California eugenicists and their connections to Nazi Germany, despite both of us having grown up in the Bay Area and gone through undergraduate education in the UC system. We must be aware of this racist history in order to challenge its current implications in the institutions that we are a part of. I am grateful to the JMP for allowing me to integrate critical race theory into my medical education through sessions like this one, and I feel a responsibility to share what I have learned.
—Second-year medical student
The conceptualization of race as biology is rooted in colonization.
Race began to emerge in society as a function of colonization, as European colonizers began encountering natives and importing slaves who looked different than themselves. Scientific racism emerged from theories of biological inferiority, including Carl Linnaeus’s polygenism (the belief that humankind evolved from two or more distinct ancestral types or races) and Dr. Samuel Morton’s efforts to compare cranial capacities of white colonizers, native people, and enslaved people. These flawed theories cemented societal conceptions of skin tone differences and nonwhiteness as biological concepts. The consequences of such frameworks during colonization and slavery resulted in the foundations of race as we know them today:
With slavery, however, a racially based understanding of society was set in motion which resulted in the shaping of a specific racial identity not only for the slaves but for the European settlers as well. Winthrop Jordan has observed: “From the initially common term Christian, at mid-century there was a marked shift toward the terms English and free. After about 1680, taking the colonies as a whole, a new term of self-identification appeared—white.”60
Such historical context laid the groundwork for racial inequality, including the expropriation of property from natives, denial of political rights, slavery and other forms of coercive labor, and explicit extermination and lynching of nonwhite people.
A clear thread can be drawn from the scientific racism of scientists like Linnaeus and Morton to institutionalized racism in science and medicine today. Considered the “father of taxonomy,” Linnaeus’s initial publication, Systema Naturae, in 1735, classified four “varieties” of human species: Americanus, Asiaticus, Africanus, and Europeanus. The classification system claimed Eurocentric superiority through the characteristics ascribed to each race: “Native Americans as reddish, stubborn, and easily angered; Africans as Black, relaxed, and negligent; Asians as sallow, avaricious, and easily distracted; while Europeans were depicted as white, gentle, and inventive.”61 The classification system was then used to “validate” European subjugation of “lower” races.
Similarly, in his 1839 publication, Crania Americana, Morton put forth race-based interpretations supporting white superiority, racial hierarchy, and Black inferiority through his calculations of marked differences in cranial capacity and brain size. His conclusions were praised for their scientific rigor and used to provide a moral justification for slavery. Scientists who followed Morton’s ideologies of different human races being different human species were considered a part of the “American school.” In 1981, Stephen Jay Gould challenged Morton’s work, exposing inherent biases and flaws in data collection, analysis, and reporting.62 While Linnaeus and Morton’s work has been repeatedly disproven, the categories of race in such research continue to be taught without critical analysis of their historical origins of racism.
Although Morton died eight years before Charles Darwin published Origin of Species, Morton’s colleagues in the “American school” used Darwin’s revolutionary theories of evolution to perpetuate their theory of social Darwinism.63 Social Darwinists applied Darwin’s theory of “survival of the fittest” to humans, claiming that certain groups of people were “less fit” than others, and therefore less deserving of survival. New scientific theory was appropriated for racist social ends, and the social category of race was biologized to justify social hierarchies.
As these worldviews began to popularize and become normalized in scientific and everyday discourse, it paved the way for the eugenics movement of the twentieth century. Eugenicists repeated the arguments of social Darwinists before them. In both Europe and the United States, eugenicists aimed to encourage the reproduction of more “fit” races and extermination of those who were “biologically inferior”:
Eugenics was the pseudoscience aimed at “improving” the human race. In its extreme, racist form, this meant wiping out all human beings deemed “unfit,” preserving only those who conformed to a Nordic stereotype.64
Medicine must recognize that the eugenics movement played a central role in the history of race-based science. In the United States, eugenics took the form of forced sterilization, segregation, and antimiscegenation laws, all specifically aimed at the extermination of nonwhite people. In Germany, Nazi doctors practiced eugenics by slaughtering, torturing, experimenting on, and murdering millions of people.65 The perpetrators of these crimes were trained physicians and often distinguished scientists, who were inspired and actively influenced by eugenicists in the United States. Adolf Hitler is recorded telling another Nazi, “I have studied with great interest the laws of several American states concerning prevention of reproduction by people whose progeny would, in all probability, be of no value or be injurious to the racial stock.”66
While their names are little-known, American eugenicists included race scientists on the University of California Board of Regents, and funding for their work came from corporate philanthropies like the Carnegie Institution and the Rockefeller Foundation. Organizations as well as individual doctors in the United States came up with their own “solutions” to exterminate inferior populations. For example, the Carnegie-supported 1911 “Preliminary Report of the American Breeders’ Association to Study and to Report on the Best Practical Means for Cutting Off the Defective Germ-Plasm in the Human Population” proposed eighteen “solutions,” including euthanasia.
When World War II ended, eugenics was declared a crime against humanity. During the Nuremberg trials, Nazi doctors and experimenters cited the influence they received from American eugenicists, but the Americans were not prosecuted. Instead, some of the exact same American scientists renamed their cause “human genetics.” They continued to collaborate with former Nazi eugenicists who had similarly avoided prosecution. For example, Otmar Freiherr von Verschuer, who founded a eugenics facility in Frankfurt, Germany, in 1935, reestablished his connections with California eugenicists from before the war and became a corresponding member of their newly founded American Society of Human Genetics in 1949.67 This legacy underlies the practice of genetics and race-based medicine today.
In calling out this legacy, we do not claim that genetics and eugenics are equivalent. Instead, we call on clinical practitioners, researchers, and instructors to recognize the history that seeks to reappropriate agendas of racism and eugenics in more “neutral” terms that still have historical and contemporary ramifications. Uncritical use of race in genetics and other aspects of medicine stands to perpetuate causes of racism and inequality.
The flawed assumption that race has a biological basis is rooted in a racist history dating back to colonialization and slavery. With this history, we emphasize: race is not a biological concept, but rather a sociohistorical construct and concept. Under this definition, racial categories have no scientific basis but have rather functioned as a central axis to social relations and real material life outcomes in the United States.
Section 3: Race-Based Medicine in Diagnosis and Treatment
In multiple medical textbooks (such as Robbins and Cotran) and popular health reference websites (such as Medscape, WebMD, UpToDate), I have seen race as a risk factor in disease and pathology, particularly among Black and Hispanic/Latinx communities. Whether it’s hypertension, kidney failure, interstitial lung disease, asthma, diabetes, and more…the medical community has cemented one’s race as a biological destiny and of inherent biological danger. This framing misses the point: Racism, not race, is a risk factor.
—Third-year medical student
The concept of race has no biological basis. Racism, not race, has been and continues to be a key determinant of health outcomes, especially in the United States. Research that falsely biologizes race dates back to colonialization and slavery, and contemporarily translates to poor clinical guidelines. And yet, medicine continues to uphold the idea of biological race—and, thus, racism—in diagnosis and treatment schema.
What does this look like in context? Clinicians will use a patient’s skin color and ethnicity as heuristics to determine their diagnosis and treatment plan. In fact, race serves as a shortcut for clinical thinking from the onset of training, as evidenced in the United States Medical Licensing Examination.
A study question tweeted by the American College of Obstetricians and Gynecologist (@ACOGAction) reads,
A 33-year-old married African American woman comes to your office and admits to thoughts of suicide for the last month. She was previously diagnosed with bipolar disorder, but has never attempted suicide before. Which of the following characteristics is associated with an elevated epidemiological risk for suicide? The listed options are A. Age < 35, B. Bipolar disorder, C. Lower socioeconomic status, D. Being married, and E. Black race.”68
Although the correct answer, according to the ACOG, is B. Bipolar disorder, question writers likely included “Black race” as an option because they thought test takers would rely on the pervasive, yet false, assumption that race is an epidemiological risk factor for various pathologies.
Another test prep resource offers the following on sickle cell anemia:
Sickle cell disease (SCD) is a multisystem disorder and the most common genetic disease in the United States, affecting 1 in 500 African Americans.69
Robbins and Cotran Pathologic Basis of Disease, one of the foremost pathology textbooks for medical students nationwide, offers this epidemiologic look at sickle cell disease:
About 8% to 10% of African Americans, or roughly 2 million individuals, are heterozygous for HbS….There are about 70,000 individuals with sickle cell disease in the United States. In certain populations in Africa the prevalence of heterozygosity is as high as 30%.70
Both sources pathologize—and racialize—African Americans as the only potential population for sickle cell anemia. This risks missing diagnoses in other populations or oversimplifying clinical reasoning for African Americans.
Yet another test prep blog offers this summation:
Board questions reflect an extremely judgmental worldview with heavy-handed generalizations about race, sex, and a wide variety of stereotypes. African American females in their 30-40s have sarcoidosis.71
Race is thus used as a tool to expedite not only test questions but also diagnostic processes. Frankly, this shortcut can be dangerous and inaccurate. For test questions, this enforces racial bias that may be present or introduces new ones.72 This translates directly to clinical care, where a patient’s race is seen as a risk factor for disease and requires that providers associate certain illnesses with certain races. As such, providers may never inquire into the root causes of illness for a person experiencing racism and inequality (such as structural and social determinants of health) or may miss more complicated and nuanced diagnoses. Furthermore, they may overlook diseases in patients of races and ethnicities that are not traditionally associated as “risk factors.” For example, sickle cell is thought of exclusively as a Black(-only) disease and thalassemia as a Mediterranean(-only) disease. Cystic fibrosis is underdiagnosed in populations of African ancestry because it is thought of as a white disease.73
In the following section, we provide examples of how health care and biomedical research conflate race with biology. We discuss the racist underpinnings of the diagnosis and treatment of heart, kidney, and lung disease. We also explore faulty science that reifies biological race within precision medicine. If medicine is to help alleviate racial health disparities, we need to eliminate these embedded heuristics and false assumptions while addressing social and structural determinants of health.
Heart Disease
One day in clinic, my preceptor asked me to counsel a patient on cardiovascular disease risk and prevention, using the Atherosclerotic Cardiovascular Disease Risk Estimator provided by the American College of Cardiology. I spun the computer screen around and filled it out with him. Age, sex, then suddenly “race,” and the only options were “white,” “African American,” and “other.” I was confused. Even he was confused. “Why is this relevant?” he asked me. “And as a Spanish-speaking immigrant,” he went on, “what would I be?”
—First-year medical student
Black people disproportionately experience cardiovascular disease in the United States.74 Research on allostatic load and stress finds discrimination—resulting from internalized, interpersonal, institutional, and structural racism—to be an arbiter for poor cardiac health among Black people in the United States.75 Health disparities are consistent across multiple outcomes known to be markers for cardiovascular disease: hypertension, subclinical carotid disease, coronary artery calcification, coronary artery obstruction, elevated cholesterol, visceral abdominal fat deposits, and increased C-reactive protein.76
However, despite this research, clinical guidelines for diagnosis and treatment of cardiac disease do not take discrimination or structural factors into account. Instead, they attribute the cause of disproportionate outcomes to one’s race alone. For example, the following guideline is from the Eighth Joint National Committee, which sets national recommendations on treatment thresholds, goals, and medications in the management of hypertension in adults: “Initial antihypertensive treatment should include a thiazide diuretic, calcium channel blocker, ACE inhibitor, or ARB in the general nonblack population or a thiazide diuretic or calcium channel blocker in the general black population.”77 Furthermore, angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers are recommended as first-line agents only in Black people with comorbid chronic kidney disease.78
Here, Black or African American racial identity is treated as a proxy or a unique numeric variable for diagnostic equations and treatment indications. The use of Black racial identity as a proxy appears in claims ranging from increased “salt sensitivity” contributing to hypertension and the supposed need for specialized pharmaceutical treatments (e.g., BiDil). Use of racial identities as sole determinants of health outcomes frames Black people as having “inherently” poor cardiovascular health.
Framing racial disparities in cardiovascular disease as a product of the social category of race itself is harmful because it falsely attributes racial disparities to genetics and other underlying biological characteristics and it ignores the contributions of internal, interpersonal, institutional, and structural racism to these disparities.
Hypertension—Salt Sensitivity Hypothesis
Many clinical researchers and medical providers today are aware of the Black health disparities in hypertension, oftentimes with many thinking that such disparities are a result of genetic or biological predisposition. However, few clinicians are aware that these assumptions are erroneous and originated in misguided assertions of the “African gene” hypothesis, in which Black people are more likely to have salt sensitivity as a by-product of the slave trade.79 This assertion is further misguided as critical theorists have pointed out that no current or contemporary West African populations suffer rampant hypertension. Despite this, the American Heart Association website declares: “Researchers have also found that there may be a gene that makes African Americans much more salt sensitive.”
On Medscape and WebMD, two popular publishers of medical information for the general public, cursory searches on the intersections of salt sensitivity and Black race argue that “high rates of high blood pressure in African Americans may be due to the genetic makeup of people of African descent. Researchers have uncovered some facts: In the United States, Blacks respond differently to high blood pressure drugs than do other groups of people.”80 Claims of biological racial differences in salt sensitivity have unclear origins. In a recent paper by Lujan and DiCarlo (2018), the authors note that “Wilson and Grim…published only a single peer-reviewed scientific paper on the Slavery Hypertension Hypothesis in 1991. As noted by Kaufman and Hall…the majority of the written work on the slavery hypertension hypothesis is limited to conference reports and nonreviewed abstracts and book chapters.”81
In 2005, media attention praising Harvard economist Ronald Fryer’s work on salt sensitivity began to influence clinical researchers of racial difference today. It was during this time when changes to clinical guidelines associating Black racial identity with salt sensitivity popularized in clinical medicine. In the seminal paper entitled “Racial Differences in Life Expectancy: The Impact of Salt, Slavery, and Selection,” Fryer et al. hypothesizes how specific factors in the slave trade experience could explain the hypertension disparities among Black people in the United States.82 They use a Darwinistic “bottleneck theory” of evolution, in other words claiming that the catastrophic population-wide effect of slavery led to the evolutionary selection of a trait that improved survival during the Atlantic Slave Trade. In making this claim, they cite data sources, such as precipitation data and historic images of “a slave trader licking a slave’s face to assess his fitness for the voyage across the Atlantic”:
As T. Buxton writes, “…nobody suffered more intensely from thirst than the poor little slaves, who were crying for water…Perspiration is one source of dehydration….”
In a setting of profuse water loss, the ability to retain salt and hence water substantially increased the chances of survival. Contemporary accounts indicate that at least some slave traders were aware of this, and selected slaves on the basis of the salt on their skin. Figure 2 captures a slave trader licking a slave’s face to assess his fitness for the voyage across the Atlantic. Most of the selection on the basis of salt sensitivity was likely unintentional, however. Salt depleting environments and diseases were ubiquitous throughout the slave trade, favoring individuals able to retain salt (33).83
Despite Fryer et al.’s false and limited arguments to support the slavery hypothesis, this work attracted popular media attention, such as forming the basis of the New York Times’ 2005 article, “To a Unified Theory of Black America.”84 In 2007, Dr. Oz appeared on the Oprah Winfrey Show and asked the audience, “Do you know why African Americans have high blood pressure?” to which Winfrey studiously replied, “African Americans who survived [the slave trade’s Middle Passage] were those who could hold more salt in their body,” with Dr. Oz’s enthusiastic agreement.85
With the widespread blind acceptance of the salt sensitivity hypothesis among clinicians, hypertension disparities faced by Black people are seen not as a consequence of stressful environments and situations caused by social and structural determinants but rather by false notions of biological differences in salt retention. As noted by critical race theory scholar Osagie Obasogie, perhaps the most important rebuttal to the hypothesized link of salt retention and racial difference is the fact that “no contemporary West African population suffers from rampant hypertension. Historical records suggest that Africans’ overall mortality during the Middle Passage was about 13 percent. For a bottleneck theory to hold up, the alleged ‘salt sensitive gene’ would have had to play a significant role for the roughly 87 percent that survived, implying that this gene was relatively common among enslaved West Africans.”86
False notions of salt sensitivity that are currently present in clinical medicine and practice will continue to inflict harm on Black communities, as such bad science deflects from attention to social, structural, and environmental stressors that are linked to susceptibility and exacerbation of hypertension.
BiDil
The implications of the erroneous correlation of Black racial identity with hypertension have not only affected clinicians’ perception of disease and pathophysiology, but also treatment for Black people. In 2005, BiDil, a combination pill of two standard therapies—hydralazine and isosorbide dinitrate—for heart failure, became the first drug to receive approval from the US Food and Drug Administration (FDA) to treat a specific racial group—African Americans.87 However, the clinical development of BiDil was never intended for an explicitly racialized purpose—it was simply another drug to treat heart failure. In this section, we will reveal how the drug development of BiDil is an example of bad science and epidemiology. Moreover, we will explain how the development of BiDil predicated on the use of ideas of the biological inferiority of Black people in order to gain commercial and market success.
In the 1980s, cardiologist Jay Cohn led two clinical trials—V-HeFT 1 and V-HeFT II—to study the drug. The investigators of these trials, however, “did not build the trials around race or ethnicity. They enrolled both Black and white patients and in the published reports of the trials’ successes, they did not break down the data by race. Rather, they presented BiDil as generally efficacious in the population at large, without regard to race and filed a patent.”88 However, despite these assertions, the FDA rejected BiDil’s approval due to statistical design flaws in these trials in 1997.89
The FDA rejection did not restrict use of data from the V-HeFT trials. In an attempt to reconsider how to best market the drug to the FDA and public, Cohn, along with his coinvestigators, returned to the V-HeFT data and recategorized the results by race. There was no scientific reason for this reanalysis, for Cohn and his coinvestigators only turned to race after the initial application to market failed for commercial purposes. In 1999, nearly fifteen years after the first V-HeFT 1 data was collected, the investigators claimed they had discovered a race-based differential response to BiDil treatment.90 Then, Cohn “filed for and was granted a patent identical to the first one, except that the use was now for African Americans suffering from heart failure, which had the financial and commercial benefit of extending his patent rights an additional thirteen years.”91
A company named NitroMed gained the license for BiDil from Cohn and conducted a new clinical trial, the African American Heart Failure Trial (A-HeFT), in order to test BiDil’s race-specific benefit. However, this new trial only included participants that self-identified as African American and did not include a comparison group. Therefore, the trial could not have demonstrated that BiDil works better in African Americans than in any other group. As a result, this specious “reanalysis” opened the door for an epidemiologically flawed race-based trial. Despite this fundamental design flaw, the A-HeFT trial produced data “demonstrating a 43 percent reduction in mortality, leading the FDA to approve a race-specific indication for use by Blacks with heart failure.”92 Neither Cohn nor any of his collaborators have been able to identify the biological markers responsible for Blacks’ receptiveness to BiDil. Cohn himself states that the drug is effective in non-Black patients as well. The same year that BiDil gained FDA approval, Cohn admitted to prescribing the generic drugs constituting BiDil to 25 percent of his white patients.93 He directly stated, “I actually think everybody should be using it.”94
Ever since its FDA approval, BiDil has been widely prescribed in a race-specific manner, based on the prevailing yet unfounded assumption that “self-identified race mirrored some underlying ‘real’ biological difference that shapes health disparities and drug reaction.”95 As medical students, we are implicitly taught the same assumption through uncritical textbooks and precepting clinicians. A widely used pharmacology textbook directly states, “A fixed combination of hydralazine and isosorbide dinitrate is available as isosorbide dinitrate/hydralazine (BiDil), and this is currently recommended for use in African Americans.”96
The race specificity of BiDil is unsubstantiated and commercially motivated, yet “it has come to reflect the legal, regulatory, and economic sanctioning of race as a biologically significant category of human difference that meaningfully affects human health” [Obasogie]. This framing falsely leads social categories of race to be perceived as the causes of disease and for structural causes of disease being ignored. Critical race legal scholar Dorothy Roberts powerfully summarizes,
While the racial gap in life expectancy widens, owing largely to the government’s failure to address structural inequities, the poor health of African Americans opens new markets for pharmaceutical companies. The claim that race-based biotechnologies will shrink the gap based on genetic difference is a powerful way to deflect concerns about their unjust social impact and the social inequality that actually drives poor minority health. We should be against an approach that promotes individual health through technological cures as a way of ignoring larger social inequities. This view sets up a false dichotomy between health and social justice: it treats health and justice as opposing values, weighs them against each other, and declares health the winner. It hides the social factors that determine health not only for individuals but for the entire nation. Letting health trump social justice does not really improve the welfare of most people; it supports the interests of big business and the most privileged members of society.
The promotion of race-based medicine misrepresents the relationship between genes, drugs, and health disparities. Of course, pharmaceuticals can help improve sick people’s health, and effective pharmaceuticals should be available to people who would benefit from them. But health inequities are not caused by genes and cannot be eliminated with drugs. Promoting race-based medicine with the myth that poor minority health is caused by genetic difference will only widen the gap, diverting us from the real solution. It makes no sense to put aside social justice concerns in order to improve minority health. A more just society would be a healthier one.97
Kidney Disease and Glomerular Filtration Rates
A faculty nephrologist at our school was talking to us at an event about the issue of using race so visibly in GFR rates. She noted that when alternative corrections were suggested, like having physicians estimate muscle mass instead, other physicians “freaked out” and asked her how they could possibly accurately measure a person’s muscle mass “just by looking.” She asked us, “Why are we so much more comfortable assigning someone a race, and differentiating their treatment based on that, than we are about estimating muscle mass?” I realized how blind I’d been to all the times my preceptor and other providers I worked with were assigning race to patients and adjusting their care accordingly.
—Second-year medical student
National and international studies show racialized disparities in chronic kidney disease (CKD) and end-stage renal disease (ESRD), the terminal stage of CKD.Unknown Object CKD has been named an important contributor to both national and global morbidity and mortality, with a vastly disproportionate burden falling on people of color. In America, as of 2013, although the rates of CKD were relatively comparable, Black people had four times the rate of progression to ESRD than non-Hispanic white people.99 The reasons behind this are complex, with structural factors at the forefront—lack of access to care, environmental toxins, chronic stress, and poverty—all highlighted by Nicholas et al.100
Biologically, kidney disease is intimately related to heart disease. Hypertension, or high blood pressure, is a leading cause of CKD, and Black people in the United States have a seventeenfold higher rate of hypertension as the etiology or cause of their ESRD than other populations.101 102 An underdiagnoses of hypertension in Black people due to the previously mentioned clinical racism may thus also contribute to disparities in kidney disease, putting Black people at risk for long-term, severe kidney damage. But there are other, more direct issues.
Biological racism is embedded in a key tool used to measure kidney function—the glomerular filtration rate, or GFR. The GFR is a calculated measurement of a particular protein in the blood that the kidneys filter, which is then used to estimate kidney function because kidney function can’t be measured directly in a typical clinic. It provides clinicians with an approximation of how well the kidneys are performing their critical roles of filtering fluid in the body. The GFR is used to diagnose many kidney-related diseases, including CKD. It is thus especially important for classifying severity of CKD (up to and including ESRD) and for making decisions about diagnosis, prognosis, and treatment of kidney disease. Embedding biological race in this tool leads directly to a deadly underdiagnoses of severe kidney disease in Black people, contributing to the disparate epidemic of ESRD and CKD seen today.
The GFR is currently estimated through complex equations that take into account individual factors, including weight, age, sex, serum levels of creatinine (a waste product from muscle breakdown that is excreted in urine), and race. Based on these equations, the further someone’s GFR is below “normal,” the increased severity or stage of kidney disease. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) is the most commonly used equation and was developed in 2009 as an improvement to the 1999 Modification in Diet for Renal Disease (MDRD) study equation.
These two commonly used equations—CKD-EPI and MDRD—each contain a racial adjustment factor coefficient that is multiplied to the baseline GFR estimate for a Black person (1.16 for CKD-EPI; 1.21 for MDRD).103 This adjustment increases the GFR for a Black person for a given creatinine level in both equations, which means the adjusted GFR is closer to normal and thus creates a diagnosis of a lower disease severity. Compared to a white man of the same age, weight, and serum creatinine level, the estimated GFR of a Black man would be higher, suggesting that Black people have “better kidney function” than individuals of other races. Because of this, Black people must meet higher GFR thresholds of kidney function in order to be diagnosed with kidney disease compared to individuals of other racial groups.
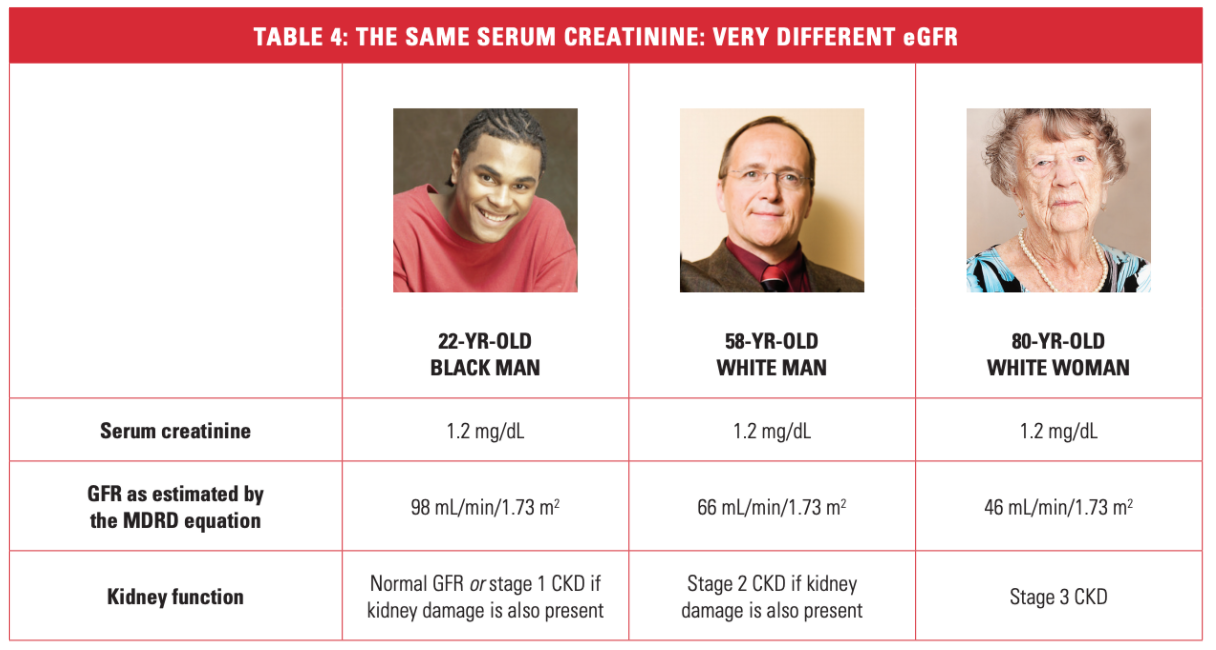
Image source: “Frequently Asked Questions about GFR Estimates,” National Kidney Foundation104
This racial adjustment factor has severe negative clinical implications. Those who identify as (or are identified by their providers as) Black may not be diagnosed early enough, may not receive intervention at a critical period, and are more likely to progress to higher stages of kidney disease and poor health outcomes.105 The racial adjustment means it takes worse kidney function to get diagnosed with CKD for Black people, and by the time they are diagnosed, they are often at ESRD (CKD is classified as stages 1–5, with ESRD being stage 5). Studies show a two- to fourfold higher incidence (counts of new cases) of ESRD among Black patients as compared with white patients.106 Yet the prevalence (new cases plus existing cases) of earlier stages of CKD in Black patients is similar or lower than that of white patients, meaning the GFR adjustments may be delaying diagnosis of earlier-stage CKD until Black patients have reached a significantly higher disease burden and are already at ESRD.
Other biological markers beyond GFR help the classification of CKD stages and ESRD, so we would expect those markers to match across CKD staging for different populations if the GFR measurement were accurate. However, white populations with stage 3 CKD display a strikingly lower prevalence of other risk factors for CKD, such as albuminuria and hypertension, compared to the Black populations.107 This evidence suggests that either white patients are being diagnosed with more severe disease than they actually have or that Black patients are being diagnosed with less severe disease than they actually have. Given the current race coefficients in measuring GFR, this evidence suggests that clinicians may systematically misclassify disease status among Black people to a falsely lower CKD stage (Peralta 2010). Despite having known risk factors for CKD, such as albuminuria and hypertension, young Black people may only be diagnosed once they reach advanced stages of disease.
This all adds up to a disproportionate disease burden. Black patients represent 30 percent of all ESRD patients in the United States, and just 13 percent of the total US population.108 The only cure for ESRD is a kidney transplant, yet Black patients are less likely to be identified as transplant candidates, more likely to be on waiting lists for longer, and less likely to receive a deceased or living kidney donation compared to white patients due to both institutional and structural factors.109 Not only is the current race-based system of determining GFR scientifically flawed, but it actively harms Black patients by systematically missing early diagnoses of CKD.
These dire health implications beg the question, Why do racial adjustment factors exist for GFR at all? The National Kidney Foundation states that race is included in CKD-EPI and MDRD equations because “African Americans have a higher GFR than Caucasians at the same level of serum creatinine.”110 However, this argument is somewhat circular and has many scientific limitations.
The MDRD and CKD-EPI equations appeared in 1999 and 2009, respectively, to improve upon an older equation (Cockcroft-Gault formula) developed in 1973 with a cohort of 249 men. The 1999 MDRD equation was then reformulated in 2005 (right at the time that the research in salt sensitivity was spiking), and the CKD-EPI was created shortly after that. Each equation represents an academic “doubling down” on race in the name of improving the accuracy of estimating kidney function.
First, the demographic profile of each study was crucial to the specific equation development, and often not representative of the United States (e.g., there are generally fewer people of color in the study as a percentage than the percentage of the US population—the MDRD study was 88 percent white). Therefore, extrapolations about the creatinine clearance for more diverse populations along any of the parameters used in the equation are bound to be of limited use.111 For example, age is a key factor in the equations, and the dataset for MDRD only included older people (average age 50.6) with CKD, which, therefore, may not apply to healthy populations, particularly younger populations. One study showed this was particularly true for young Black people, who may be significantly misclassified with lower or no CKD.112 And because the formulas were derived from American, mostly white populations, their utility may be limited for multiethnic populations especially in other geographies. A study of multiethnic Brazilian populations showed CKD-EPI has similar accuracy to MDRD regardless of race corrections when compared to the gold-standard direct measurement of GFR function, iohexol clearance.113
Second, creators of both the CKD-EPI and MDRD equations do not provide sound evidence for why race was included in the model for calculating GFR in the first place. The authors of the MDRD equation did not include an explanation in their methods for why they included race in their model. In their conclusions, they simply state, “on average, black persons have greater muscle mass than white persons.”114 The evidence base for this assumption is fundamentally flawed. The three studies the MDRD researchers cited to support their claim were fraught with questionable scientific methods regarding race, including “visual determination” of study participants’ race categorization and grossly racist “anthropometric measures” such as “densitometry” to generalize questions of overall muscle mass across races (Levey et al. 1999; Cohn et al. 1977; Harsha et al. 1978; Worrall et al. 1990).115 Harsha’s densitometry results are unlikely to hold up today, as he posited that Black children on the whole had much less body fat, while today children of color are far more likely to be obese. This points to the racist assumption that these characteristics were biological instead of structural or societally influenced. The creators of CKD-EPI, which was meant to improve upon MDRD, included race simply based on the fact that MDRD did.116
Furthermore, the race categories represented in the equations are arbitrary and do not reflect the heterogeneity of human populations. They reflect the social categories that society has designed, based on arbitrary visual and social standards. The MDRD study never explains how it classified participants by race nor how it defined race, while the CKD-EPI only notes their source data was the National Health and Nutrition Examination Survey, which tends to use self-identification within the given options. These options are typically drawn from the census options, which are both socially constructed and confusing by conflating race with ethnicity. As an example of the limitations of these arbitrary definitions of race, Zanocco’s study of a multiethnic Brazilian population showed that the race adjustment was not associated with better performance in evaluating GFR, demonstrating that it is not a necessary or useful tool in multiethnic populations.117 Further highlighting the arbitrariness of the racial categories used in calculating GFR, nephrologists have anecdotally admitted to misidentifying patients as African American based on their brown skin, meaning their understanding of the usefulness of the GFR equation is based on visual assumptions.118 This questions the scientific usefulness of such GFR estimations and highlights the racism inherent at every level of the interaction, from the structural construction of the flawed GFR equation to the interpersonal racism of misidentifying patients based only on skin color.
Third, the equations take into account several biological factors such as age and gender alongside (nonbiological) race, but do not include muscle mass. Muscle mass is crucial in the GFR calculation because creatinine, one of the main serum markers, is a by-product of muscle breakdown. Thus, those with higher muscle mass and those with poor kidney function would both have elevated serum creatinine levels, leading to lower estimated GFRs. The National Kidney Foundation guidelines themselves explain that the estimated GFR calculations are less accurate for patients who do not have an average muscle mass and standard diet, including athletes, people over seventy years old, the malnourished, the obese, vegetarians, or patients with changing kidney function.119 Although the biological mechanisms by which these factors affect muscle mass are well understood, only age is “adjusted” for in calculating GFR.
However, the variable of race is adjusted for, not muscle mass, and often anecdotally referred to as a proxy for muscle mass without any explanation for why race would be related to muscle mass. A quick Google search will turn up hundreds of papers seeking to justify or explain differences in body habitus (e.g., muscle mass, body mass index, adiposity) with biological mechanisms that are then explicitly or implicitly tied to a biologized notion of race. These papers either ignore social and structural determinants of health (e.g., ignoring the effect that lived experience and environment may have on body composition) or have a blatantly racialized research agenda seeking to uphold a preconceived notion that racialized biological differences exist.120 Although differences in bodies do exist across different people, the differences are far more nuanced than the social category of race. These notions underscore the existing racist perceptions and stereotypes about Black physicality that links to the historical positioning of Black “fitness” for manual labor, and has continued today through stereotypes about Black athletes, among many others.121 The linkage of muscle mass to race has historical roots and is fundamentally rooted in racism.
If muscle mass is a key factor in calculating GFR, an estimation of muscle mass itself should be included in the equations. If it is not yet easy to measure in clinic, then we should create better tools to measure it. Race should not be crudely and harmfully used as a proxy for muscle mass.
As Dorothy Roberts explains in her TEDMED talk, “The Problem with Race-Based Medicine”:122
But what sense does it make for a doctor to automatically assume I have more muscle mass than [a] female bodybuilder? Wouldn’t it be far more accurate and evidence-based to determine the muscle mass of individual patients just by looking at them?…Race is a bad proxy. In many cases, race adds no relevant information at all. It’s just a distraction. Race also tends to overwhelm the clinical measures. It blinds doctors to patients’ symptoms, family illnesses, their history, their own illnesses they might have—all more evidence-based than the patient’s race. Race can’t substitute for these important clinical measures without sacrificing patient well-being.
Finally, the racial adjustment factor in GFR estimates can also be directly harmful to patients of color through psychological impacts. “Separating out one ethnic group from the general population on a laboratory slip” can lead to stigma and other interpersonal or internal forms of racism, as well as potentially delaying diagnoses.123 The psychological impact of false-positive tests is routinely discussed in the usefulness of screening tests for cancer, and although the GFR adjustment is a question of “false-negative,” every clinical field should be held to the same standard to “do no harm” through the psychological impact of how test results are displayed and discussed.124
As medical students, we are taught to follow the CKD diagnosis algorithms, which hide much of the reliance of race in GFR calculations, and we are implicitly taught to accept that Black patients simply have a higher disease burden. However, the reality of this is a direct repercussion of using race as an inappropriate heuristic, one that has dire health consequences for Black patients.
Lung Function, Spirometry, and Current Recommendations by the American Thoracic Society
Danielle M. is a patient at her local hospital coming in for a checkup with her doctor regarding difficulty breathing over the past few days. As her doctor is preparing for her visit, she looks at the information stated in the electronic medical record:
-
Gender: Female
-
Age: 50
-
Reason for visit: Difficulty breathing for the past month
-
Language: English
-
Race/Ethnicity: Black/African American
-
Smoker: Yes
With these demographic “clues” from Danielle’s electronic medical record, the doctor arrives at the reasoning for possible differential diagnoses to discuss with Danielle: chronic obstructive pulmonary disease (COPD) and asthma. The physician plans to perform a spirometer test, a method of assessing lung function by measuring the volume of air the patient is able to expel from the lungs after maximal inspiration. Spirometry is the primary method that clinicians use to evaluate lung function. Spirometry reports include a set of values based on the patient’s volumes of inspiration and expiration, and these values are compared with a range of volumes considered to be normal.
For Danielle, the pulmonary lung function test results did not result in a clinical diagnosis, because her spirometry results were within normal limits. “Ethnic” correction factors were applied to calculate these normal limits, and Danielle’s lung function test results may have resulted in a clinical diagnosis without them.
Danielle’s doctor tells her that they’ll have to have a number of follow-up visits and additional lab testing in order to confirm her diagnosis. Danielle departs from the doctor’s appointment disappointed and nervous that her breathing continues to be labored and difficult and that it will take several more appointments to find out what is going on. She is unable to make appointments in the upcoming month due to family obligations and her hectic work schedule. Afterward, a medical student asks Danielle’s doctor if race correction factors could have impacted Danielle’s spirometry results. She replies, “Black people are always diagnosed and overmedicated. Thankfully these correction factors help with that.”
This anecdote is adapted from a true interaction one medical student had during a session with her preceptor. As medical students, we often hear statements like the one Danielle’s doctor made, where biological race is framed to us as a solution to health disparities. This framing makes it difficult to disentangle the insidious and harmful ways that the ingrained notion of biological race impacts patients like Danielle. However, challenging the notion of race as a biological trait should not be mistaken as advocacy for color-blind medicine. We want to be a part of medical practice that engages in antiracist medicine, not color-blind medicine. We advocate for medicine to acknowledge the role that flawed assumptions regarding biological race play in perpetuating racial health disparities.
This advocacy is vital because, as we show in the following example, race is dangerously built into algorithms that determine lung function, just as with kidney function. What could be considered “normal” function for Black people is repeatedly considered pathologic or unhealthy for white people. This discrepancy leads to late diagnoses and poorer treatment for Black people compared to their white counterparts.
Furthermore, the notions that racial and ethnic differences in lung capacity exist, and that these differences should be programmed into the diagnosis of lung disease, are fundamentally rooted in a history of racism. Next, we will elucidate this racist history, drawing largely from the critical work of Lundy Braun, including her book Breathing Race into the Machine.
Interest in modern spirometers first took hold as a means of assessing the fitness of police forces and military personnel and life insurance applicants in England during the outbreak of tuberculosis in the nineteenth century.125 John Hutchinson, an English surgeon, was credited with inventing the spirometer in the 1840s and also coining the measurement “vital capacity,” after his assertion that such measurement was critical in assessing premature mortality.126
The application of Hutchinson’s spirometer quickly spread, including Samuel Cartwright’s use of spirometry on slavery plantations. Cartwright was a Southern physician and plantation owner who was the first person to use the spirometer as a tool for comparison of lung function between Black people and white people.127 In particular, he asserted that “the expansibility of the lungs is considered less in the Black than the white race of similar size, age and habit.”128 Benjamin Apthorp Gould published the first study in 1869 that would reinforce notions of biological inferiority of Black people with data on racial comparisons of lung function with large sample sizes and anthropometric measurements of Union soldiers. These assertions, alongside subsequent studies that found that slaves had poorer nutrition status and higher rates of pneumonia, typhoid fever, and respiratory illnesses, contributed to racist assertions that African American slaves had physical pathologies and thus needed to be kept under the institution of slavery.129
Political leadership who profited from the institutions of slavery, including Thomas Jefferson, reinforced the influence of notions of biological inferiority of Blacks and non-Caucasian populations. Despite taking part in asserting that “all men are created equal,” Thomas Jefferson, in his Notes on the State of Virginia, featured racial differences in lung function between white colonialists and slaves, asserting that there were marked distinctions between such groups and “a difference of structure in the pulmonary apparatus.”130
This brief history of key figures involved in the history of the spirometer illustrates how notions of biological racial difference in lung capacity and fitness related to the foundations of public health and slavery. In particular, the motivation for the creation of the spirometer by Hutchinson and its subsequent use by Cartwright and Gould to obtain scientific data claiming racial difference in lung function between slaves and colonialists was used to first assess and calculate the fitness disparities of diseased individuals in society and subsequently to achieve the subjugation of slaves and control of non-Caucasian populations. By obtaining “scientific” anthropometric information that attempted to objectively assert the biological inferiority of Black people, slavery was further justified through medical and public health institutions and methods.
Perhaps the most striking element of this history is how its roots continue to be embedded in how physicians conduct differential diagnoses and patient assessments every day due to recommended guidelines. Medicine continues to uphold racist notions of biological inferiority in lung function.
For example, the web page on UpToDate regarding spirometry states the following:
Healthy African-Americans have spirometric values that are approximately 12 percent lower than Americans of Caucasian descent of the same age, sex, and height. This difference is, in part, due to a difference in the ratio of trunk size to standing height, i.e., African-Americans have longer legs for a given height. Genetics and nutritional factors may also play a role in differences by race/ethnicity.131
UpToDate is considered an “evidence-based clinical resource” that clinicians use every single day after patient appointments for information about medications, diseases, clinical guidelines, and more. This statement by a frequently used, highly regarded medical resource is problematic for many reasons. First of all, we know that when studies use the category “African Americans,” race is typically self-identified or guessed by the clinician. To think that a statement as simplistic as “African Americans have longer legs for a given height” could possibly apply to all people who would fall into that category is absurd. Secondly, it is unclear how trunk size to standing height ratio can be emphasized as so critical in explaining spirometric values.
UpToDate cites two articles to support their claim. The first article cites another article that cites another article, and all the articles in this chain repeat the same statement without further explanation. For example, the first citation by UpToDate states, “African-Americans on average having a smaller trunk:leg ratio than do Caucasians,” and does not offer any evidence for why this observation should be singularly focused on over environmental and structural factors as a basis for correction factors in spirometry.132 The second citation by UpToDate regarding trunk to height ratio says, “Differences due to ethnicity are not well defined.”133 If the differences are so poorly defined, it is shocking how a resource so frequently used as UpToDate can so uncritically repeat that conclusion. Additionally, despite this lack of evidence, if trunk to standing height ratio really is the key factor in determining spirometric values, then race is a poor proxy for this ratio.
In practice, these assumptions about differences in lung function are built into spirometers as “race correction” factors that lead to different diagnoses for patients of different races. Anne Fausto-Sterling describes, “Technicians present spirometry results ‘corrected’ for race, so that for an African American to receive a diagnosis of impaired lung function—for example, a worker seeking disability compensation for lung damage from asbestos—he or she has to be dramatically sicker relative to a white American before receiving an equivalent disease diagnosis.”134 Here, Fausto-Sterling is referencing a case in 1999 in which Owens Corning, a company that sickened thousands of workers through its asbestos-containing products, requested that African American workers filing lawsuits against the company show that they have worse scores on lung function tests than white workers as a result of asbestos exposure in order to qualify for a trial against the company.135 Owens Corning cited “medical evidence” that Black people have different lung capacities than white people.
Currently, the American Thoracic Society (ATS) specifically recommends that the Global Lung Function Initiative (GLI) 2012 multiethnic spirometry reference values be used in North America and elsewhere for the ethnic groups represented.136 The ATS establishes standards of care relating to respiratory disorders through the publication of statements, workshop reports, and clinical guidelines that health providers and trainees across the country are expected to be up to date on. There are several issues with guidelines based off of the ATS recommendations. First, the popularly used GLI reference values are extracted from datasets of overwhelmingly Caucasian populations. In addition, GLI reference values confound false notions of biological race with environmental exposures and stressors, as the following quotation from the GLI authors demonstrates:
The well documented ethnic and racial differences in pulmonary function arise from differences in body build (such as chest size or the ratio of sitting to standing height), socio-economic status (which determines bodily development in early life and leads to secular trends in body size and pulmonary function), growing up at altitude, and possibly other environmental factors. In the present study race and ethnicity were self-reported, which may not be accurate enough for clinical purposes. Indeed, in the absence of genetic typing, predicted values in self-reported African Americans may be biased by up to 200 mL.”137
These current ATS and GLI guidelines demonstrate the blatant confusion and oversimplification of using categories of race as a means of adjusting for spirometry values. Race is not the same as ethnicity, which is not the same as body build, which is not the same as socioeconomic status, which is not the same as the environment. It cannot be used as a proxy for these structural and environmental factors, which have repeatedly been proven to directly impact lung function on their own.
Lundy Braun further elaborates on this unnecessary emphasis on racial correction factors despite greater evidence supporting how environmental factors, not race itself, mediates lung disease:
There have been scientific studies showing that people who live around high pollution areas have lower lung capacity. High pollution areas also map onto minority status. Why we have chosen both in the US and internationally to focus on race to the exclusion of social class, I can only speculate. One piece of the story is that the accumulation of scientific research around a particular idea can make it hard to dislodge. With the spirometer, having the correction factor actually built into the machine makes racial assumptions invisible.”138
The consequences of the oversimplification of structural and environmental factors into racial correction factors are that these guidelines are transferred from institutional memory into everyday physician practice that affect patients, contributing to poor treatment and diagnosis assessment for people of color and subsequent racial health disparities. Despite these concerns, the ATS fails to address any responsibility in contributing to racial health disparities by encouraging the practice of applying haphazard guidelines such as those of the current spirometry reference values according to race and ethnicity. By failing to see or challenge their inappropriate use of race and the unintended consequences of the recommendations, the ATS and the clinicians who follow such recommendations continue to perpetuate the unjust, racist framework upon which the spirometer was founded.
Furthermore, the continued presence of the racist history of establishing race-based differences in lung function within the modern-day practice of pulmonology signals how the medical community has refused to address this hidden history of racism and subjugation of Black and brown bodies. There is a profound need for this history to be interrogated, discussed in dialogue within the medical community, and incorporated into medical practice. This conversation has the potential to shift focus away from misguided notions of biological difference. Medicine must acknowledge how racism and social inequalities have had a harmful impact on health outcomes in order to address racial health disparities related to lung function.
Genetics Research, Precision Medicine, Race, and Ancestry
I was a graduate student instructor for a neuroanatomy lab in which the final task for the undergraduate students was to come up with and answer a research question using the Allen Brain Atlas. One student told me he wanted to “pick a gene associated with a disease and map it to different human races.” This wasn’t even in the scope of the project assignment—we had specifically told students that we expected them to utilize the mouse brain connectivity and gene expression atlases, not the human atlas.
But this incident highlighted to me how early in our education and upbringing “race” is ingrained in us as a biological certainty, because he assumed there would be a difference in genes and brains by race. We’re taught race as a biological cause of disease and health disparities, rather than racism. It emphasized to me how vital it is that we not only understand the health consequences of racism for our individual practices as future doctors, but also that we are able to distill, disseminate, and communicate that truth as future (and current) health educators. We must eradicate the conflation of race with biology from clinical education, research, and practice. And we must also correct this false conflation of race and biology that has spread from health institutions to education and society at large.
—Second-year medical student
Research in genetics, ancestry, and precision medicine has grown exponentially due to the Human Genome Project and advances of CRISPR technology. Precision medicine is the use of advanced computing tools to integrate data from a diverse range of health and research settings. The Human Genome Project catalogued and identified the more than three billion genes in the human genome to create a baseline “reference map” of the human genome. CRISPR refers to both the gene-editing tool (an enzyme called Cas9) and its targets (clustered regularly interspaced short palindromic repeats, pronounced “crisper”). This tool has the promise to target and edit specific portions of genes (identified by the Human Genome Project) within an organism at a level of precision unseen before, which has led to many exciting developments in biological research, biotechnology, and possible treatment for certain diseases. However, advancements in these fields have concerned many scholars, ethicists, and activists, as this research and its technologies have the potential to reinforce and expand upon flawed biological notions of race.
By seeking to identify genes that could be “cured” via CRISPR, such research runs the risk of repeating eugenicist history and simplifying the complicated role that social and structural inequalities play in perpetuating racial health disparities to a gene or set of genes.
Understanding links between genetics and disease is a major component of modern health care. However, linking race with genetics is a fundamental intellectual flaw with consequences for patient diagnosis, care, and treatment. Within medicine’s history of oppression and racism, using “race” in the field of genetics and precision medicine is inherently political with complex sociopolitical origins. Without a critical analysis of this history and the categories used to define “ancestry markers,” such research in genetics and precision medicine hold the possibility and danger of reifying biological racial difference again in a newer, shinier package.
Current research in genetics, ancestry, and precision medicine falls into this trap of continuing to biologize race by several flawed methods that are simply bad science. These include, but are not limited to, (1) using predetermined racial categories to group ancestral markers (i.e., confirmation bias of racial categories) and (2) ascribing health disparities to genetic differences rather than accounting for the complex role of social, environmental, and structural factors on epigenetics and the body.
First, using predetermined racial categories to match to group ancestral markers elides the history of the creation of race as a social construct. Furthermore, the research seeking to match genetic markers to these groups shows that ancestral markers exist, but they are not consistent across the social groups of race. Early and ongoing work in genetics has shown consistently higher in-group variability than across-group variability, thus showing no genetic loci to differentiate between racial categories.139 Thus the use of “race” in genetics and precision medicine usually relies on scientists creating arbitrary categories for groups of ancestry markers that incorrectly substantiate racial categories rather than challenge the social construct of race.
One example shows the difficulty of applying precision medicine within the existing racist history of medicine. In July 2010, the New England Journal of Medicine published “Genetic Ancestry in Lung-Function Predictions” by Rajesh Kumar et al. In this article, the authors sought to improve upon the racial classifications used in lung function tests. Existing methods utilize patients’ self-identified race (or physician-identified race) to define the normal lung function range for spirometry, so the researchers sought to identify alternative, genetically derived “normal” values. The aim was to use genetics to provide a more “objective” set of normal values. The authors argued that the self-identified racial categories were problematic because individuals are racially admixed, and limited racial categories are “crude descriptors of individual genetic ancestry.”140 That is, racial mixing is so frequent, and individuals have such complex racial backgrounds, that the self-identified racial categories establish inaccurate baselines for the lung function measurement.
Unfortunately, the research by Kumar et al. ultimately still seeks to confirm what genetic markers might show as “truer” racial categories. This work uses genetics to make a biological argument about social constructs. Although this is a step forward from crude racist assumptions discussed in the spirometry section, their research still fell into the trap of trying to match “ancestry informative markers” (single-nucleotide polymorphisms posited to represent statistically significant genetic differences among those of different ancestries) to socially constructed racial identities (individual self-identified race).
Rather than using genetics to identify markers that may predispose anyone to lower lung function, their study sought to solidify which markers could best predict lowered function for African Americans only. Without addressing the complex factors that mark lived experience (e.g., racism, structural, and societal factors) nor the racist history of the spirometer, this research begins with the assumption of difference for African Americans (again, using the social construct as the starting point for their supposedly more objective scientific approach). Therefore, the study only confirms racial biases by using genetics to try to prove some sort of inferiority in lung function (specifically in “forced expiratory volume”) in African Americans.
Other scientists have similarly sought to more precisely measure differences in lung function between racial and ethnic groups, though definitions and conclusions regarding the influence of racial categories has varied widely.141 Some researchers accept without question the outdated, yet popularized, notions that African Americans have lower lung function than European Americans.142 One study, examining the utility of multiethnic adjustment for spirometry, posits that adjustment works for some, but not all, racial groups.143 This study concluded that ancestry markers would be helpful to better explain observed lung function differences.
Kumar et al.’s research is different because it fits within a larger body of genetics work that seeks to better understand racial disparities in health.144 This is in contrast with other genetics research that excludes nonwhite participants as a means of “controlling” for race.145 Yet even research with a progressive, disparities-oriented health research goal can fall into these “traps” of genetics research.
Kumar et al., for example, seek to provide tools for more efficient and effective care for severe asthma and COPD, which they note African Americans have higher rates of both. Kumar et al. thus represents the good intentions of seeking to improve upon issues of inclusion and to better explain the disparate health outcomes seen across racial lines. But without a critical analysis of what racial categories mean, researchers with good intentions will continue to put forth bad science that uses ancestry markers to (purposefully or not) confirm racialized differences in biology or use genetics to explain away racial health disparities caused by social and structural determinants of health. For example, Parker et al. (2014) pick up on the ancestry-based claims of Kumar et al. to claim that a particular genetic marker can predict lower COPD lung function metrics for African Americans only, again reinforcing a biological “brokenness” in African Americans rather than addressing the role society and other factors may play.146 This is unlikely to be helpful in addressing health disparities as Kumar et al. intended, instead explaining away the disparities with genetic differences. Addressing health disparities through genetics and precision medicine is therefore very much a slippery slope, which is why we feel this critical analysis of racism and race is crucial to improving the science.
We offer instead two “red flags” for researchers and readers to consider as the field of genetics continues to move forward. We furthermore encourage all researchers and readers to dive more deeply into the field of bioethics, which has been grappling with the implications of this flawed science, to better understand the recommendations for change.
First, categories used to cluster ancestral markers are established by the scientists themselves, rather than by the clustering of the data, and rely on slippery definitions that are, at best, “mired in confusion.”147 Kumar et al., for example, chose to stratify their data to specifically estimate only “the percent African and European ancestry, assuming two ancestral populations.”148 This means that the major assumption on which ancestry markers are based is one of confirmation bias (assuming only African and European ancestry in this case), such that scientists’ quests to look for patterns (oftentimes with racial categories as their foundation) will be found. Scholars of race, technology, and health justice have produced significant work for decades, pushing back against the reification of racial categories. Yudell et al. write that “historical racial categories that are treated as natural and infused with notions of superiority and inferiority have no place in biology.” They write furthermore that “using race as a political or social category to study racism and its biological effects, although fraught with challenges, remains necessary” (emphasis added) to “understand how structural inequities and discrimination produce health disparities in socioculturally defined groups.”149 Other scholars, such as Duana Fulwiley, Dorothy Roberts, and Troy Duster, have argued similarly against the use of a priori categorization in genetic research.150
Second, focus on ancestral markers fails to acknowledge the role structural and societal factors play (as Yudell et al. acknowledge) and what role epigenetics thus plays in the development of structural health disparities. As expanded upon in the following section, epigenetics is the modification of gene expression, such that environmental influences can affect to what degree genetic susceptibilities and predispositions are “active” and “inactive.” Given the breadth of public health and medical literature showing how social, structural, and environmental factors affect the expression of genes, research into the genetic foundations of health outcomes must also examine epigenetic influences that factor into differences between phenotype and genotype. Any focus exclusively on genotype with no exploration of how and why certain genes are expressed and influenced by environmental and structural factors is wholly insufficient and should be questioned. The current research landscape of “ancestral identity markers” (single-nucleotide polymorphisms, also called AIMs) runs the risk of ignoring and overlooking this process, attributing focus on racial health disparities to genetic factors rather than social, environmental, and structural influences. The goal is not to practice color-blind medicine, but rather antiracist medicine that addresses all levels of racism.
Why does this matter to us as medical students? We are being taught that the newest, “best” science has the power to individualize our cures, to explain more and more of the mysteries of the human body, and yet it is still steeped in the history and context of racism in medicine. We are often caught unawares by the way educators and clinicians claim genetics as evidence of racialized differences, and this worries us for the future of our practice.
The perpetuation of biological racism in genetics research has important implications for the practice of medicine and health care. Health care is increasingly “evidence-based.” Clinicians rely on researchers to understand physiologic processes, direct innovation, and guide assessments of risk for each patient. Genetics research is, at its most functional, intended to improve health care and is characterized as an “objective” science. However, if such research fails to acknowledge its own biases based on ahistorical and racist foundations, race will continue to be biologized and discussed under the false guise and synonym of “ancestry markers,” and structural issues will continue to be hidden under those same guises.
Furthermore, the issues in genetics research create a dire future for precision medicine, the promising “evidence-based” health care of the future. Precision medicine aims to allow us to tailor treatments and diagnoses to each individual based on their unique genetic footprint. If we continue on this path of misappropriating genetic patterns to biological race, precision medicine will not only fall far short of its goal of treating individuals better, but instead will perpetuate the false notion of biologized race. This hides the social construct of race behind the same false guise of ancestry markers and could harm patients more than individualize and improve their treatment. It allows for and contributes to explicit racial profiling and stereotyping of patients and stands to exacerbate existing disparities in treatment and access to care.
Despite good intentions, such research fails to be innovative at addressing racial health disparities and instead simply “reinvents” conversations about race using the proxy of ancestry and genetics to solidify the social construct of race as falsely “objective science.”
Semantics matter in genetics research and the practice of medicine. The difference between ancestry and falsely biologized race is critical, and it’s our duty as advocates for the health of our patients, as well as creators, disseminators, and users of science, to be careful as the field of precision medicine booms. This will be the field we work in, but we are not trained to engage with it critically. Therefore, we seek to amplify the critical and difficult conversations already existing in the field of genetics in order to ensure clinicians and providers have the tools to practice critically engaged precision medicine.151
Section 4: Looking Ahead
Epigenetics: One Intersection of Biology with Sociopolitical Determinants of Health
Despite the many ways in which new scientific developments like precision medicine threaten to entrench biological racism, new fields such as epigenetics, developmental origins, and life course research are contributing to our understanding of how racism, not race, has biological effects on the body. Epigenetics and other biopsychosocial fields are pulling together biology, psychology, and upstream determinants of health to answer how racism “gets under the skin,” showing how the social and structural determinants of health (mediated or created by racism) can literally embed themselves in our cells.
Research in the developmental origins of disease has shown that the first one thousand days after conception (up to age two) is a critical period in which the developing fetus and child’s cells are most susceptible to outside influences. During this period, the fetus grows from one cell to trillions, so any early changes in these cells will be replicated and reproduced for the entirety of one’s life. Thus, exposures in the uterine environment and early childhood environment can either be protective or increase the risk of developing chronic diseases in adulthood. Literature shows, for example, that low childhood socioeconomic status both increases the physiological response to stressors and increases the reactivity to social support.152 That is, growing up poor can both increase the body’s stress response and increase the body’s ability to calm down or resists those responses in the presence of social support. Furthermore, certain exposures during this critical or sensitive period have been shown to increase the risk of type 2 diabetes, stroke, heart disease, some cancers, impaired cognitive function, and mental health issues.
The exposures posited to increase chronic disease risk in adults include environmental exposures, such as toxins and pesticides, but also “normal” or endogenous exposures produced by the mother and transmitted to the fetus in utero.153 Although the majority of literature has focused on the effects of cortisol, the stress hormone that acts as a danger signal for the growing fetus, there is also a role of environmental racism (a form of structural racism) that increases exogenous exposures. These articles posit that the more stress a mother is under during pregnancy (including overt physical and mental, as well as more subtle or everyday stressors, such as racist microaggressions), the more cortisol reaches the cells of the fetus. This is also referred to as the mother’s “allostatic load,” or amount of biochemical response to stress.
Over time, a constantly high allostatic load can cause the stress response to stay on permanently. High allostatic load impacts neuroendocrine, cardiovascular, immune, and metabolic systems, in turn contributing to various forms of damage, including cardiovascular disease, neurological atrophy, psychiatric symptoms, mortality, mobility limitations, cognitive decline, and functional impairments.154 The fetus interprets high levels of cortisol in utero as a signal that the postnatal environment will be stressful, and reprograms the developing stress response systems to stay on high alert with a short fuse, as well as inhibit the growth of some organs. This predisposes the child to increased stress-related biological damage and increases the risk of adult chronic diseases. Most importantly, as shown in section 1, the mother’s stress can be due to racist social and structural determinants of health, such as white supremacy and inequities in neighborhoods, rather than some biological aspect of their race.
A number of studies further document how racism is stressful. For example, one study at Duke University found that Black students had higher levels of salivary cortisol after learning about a violent racist crime on campus.155 Another study showed how the mere anticipation of prejudice is associated with poor physiological and cardiovascular responses.156 Amani Nuru-Jeter, a social epidemiologist at the University of California, Berkeley, further found that chronic stress from frequent racist encounters is associated with chronic low-grade inflammation.157 This literature illustrates the biological pathway through which racism leads to increased risk of adult chronic diseases.
Epigenetics, a related but slightly different field, shows similar biological causal pathways for health disparities by embedding racism’s effects under the skin. One of the major threads of current epigenetics research focuses on the body’s varied responses to stress and how these epigenetic responses, rather than inherent genetic causes, lead to racial health disparities.158 Genetics refers to the static genes inherited from a person’s biological parents, but, as noted elsewhere, these genes do not create or explain race nor many other salient physical characteristics. Epigenetics, however, are changes in the way those inherited genes are turned on or off. In other words, these are the dynamic volume controls that tell genes to amplify certain proteins while muting others, despite the same initial signal from the static genes. Epigenetics provides one mechanism by which our health and our body is dynamically created in real time by the environment inside us and outside us. More specifically, “weathering” is a term used by epigeneticists to describe how constant stressors increase allostatic load and create biochemical and cellular level by-products that wear down the body’s normal ability to regulate itself over time. Weathering may help explain racial health disparities by proposing a mechanism for the physical wear and tear of chronic stress caused by all levels of racism.159 The effects of epigenetic weathering are further exacerbated by structural factors including inequitable access to quality health care.
Darlene Francis and related researchers have shown that epigenetic mechanisms could be a key mediating process by which the social and structural determinants of health become incorporated into biochemical changes.160 This has implications for both risk and resilience to disease processes. Human development research demonstrates that many of these processes occur during the postnatal “critical period.” Epigenetic changes can be harmful, protective, or both. Other research shows implications for epigenetic changes as a link between early life (e.g., maternal stress during pregnancy) and adult health disparities along racialized lines for conditions such as hypertension, diabetes, stroke, and coronary heart disease.161 Kuzawa and Sweet note that epigenetics help explain how the effects of social-environmental exposures combine with plasticity of phenotypes (i.e., physical traits determined by genetics) in response to those environmental exposures. Most importantly, Kuzawa and Sweet make the explicit link between racism and epigenetics. Social and structural effects of racism lead to environments that affect many aspects of bodies of color.
Dr. Francis interprets this as a call to action: “If we hypothesize that racial discrimination is capable of directly altering the epigenomic profiles of genes that are important to the stress response, we can then predict that targeting and ameliorating discrimination and racism should have an equally direct, potent, and protective effect on the stress-axis epigenome.”162 Her paper “Conceptualizing Child Health Disparities: A Role for Developmental Neurogenomics” demonstrates that the social, structural, and psychological worlds in which a child is living can influence the sensitivity of a child’s stress axis during the critical period. Developmental neurogenomics, which is a hybrid of sorts between developmental origins and epigenetics research, posits a biological plasticity in early developmental life that moves away from characterizing health disparities as purely biological, purely environmental, or psychological. Instead, the effects of racism are experienced somatically as a product of immediate environment, genes, and sociopolitical context.
Epigenetics and related research provide the language and a framework for the intersection of critical race theory and biology, which should be used across clinics and research labs. It begins to elucidate how the sociopolitical effects of racism are quite literally changing the building blocks of biochemical life. This allows critical race theorists and clinicians alike to show how socially constructed race categories and racist society cause intergenerational harm on the cellular level. In other words, “critical philosophy of race should also be critical physiology of race” and vice versa.163 These fields of research show most clearly that as clinicians and researchers, we cannot engage in health without understanding both biology and critical race theory.
It is crucial to recognize that research in epigenetics and developmental origins complements but does not replace the understanding of social and structural determinants of health. Exposures at every level, from cortisol in utero up through mass incarceration, environmental racism, and white supremacy, contribute to biological risk. Thus, it is necessary and critical to clearly articulate that epigenetics does not constitute scientific evidence that Black and brown bodies are permanently damaged or broken. We as clinicians and researchers need to be loudly unequivocal that epigenetics is one line of promising research into how the many levels of racism cause biological harm, and that race is not a risk factor for disease.
This understanding of epigenetics calls on clinicians and medical educators to learn critical race theory, to become active in investigating social and structural determinants of health, and to equip themselves with the language and tools to identify racism, not race, as a cause of racial health disparities.
As medical students, we have seen that such physicians and health-care professionals are thus compelled to not only treat the medical concerns but also the structural ills in society. Our training in both medicine and critical race theory has taught us that race has no business in clinical guidelines and that the use of race in clinical guidelines is just one symptom of much larger systems of oppression. Further, the conflation of race with biology has real, negative consequences when it is incorporated into clinical practice. We are not the first to say this. Yet we seek to be physician-activists who change it. Therefore, we call on our colleagues and our educators to discontinue the use of race in guidelines as one step toward equity. We call on students, physicians, and educators to use the power of medicine to help create an equitable world in which racism no longer causes biopsychosocial harms for this generation and the ones to come.
Our Conclusions
- Medicine has willfully ignored its racist history despite ongoing calls from scholars and activists to rectify its violent and oppressive past. This has resulted in medicine continuing to inflict and perpetuate racism that harms communities of color.
- Using race as a heuristic for diagnosis of disease and interpretation of symptoms masks racism.
- Because of the biological use of race in clinical guidelines and education, patients of color are being systematically misdiagnosed and undertreated and are at risk for bad health outcomes.
- Race-based medicine teaches people of color that their bodies and communities are abnormal, deficient, and broken, increasing stress and the burden of racist stigma.
- As medicine fails to confront and rectify its origins of violence against vulnerable communities, it will continue to perpetuate an agenda that is an unwelcoming, hostile space for people of color.
If we don’t dismantle race-based medicine, it will be perpetuated.
Vision Forward
As physicians-in-training, we envision a world where the social construct of race is not conflated with biology and where the health consequences of racism are acknowledged, addressed, and cared for in all their forms.
To make this a reality, medicine must adopt antiracist institutional practices regarding research, practice, and education.
- Medicine must unveil and teach how racism has shaped scientific advancements, tools, and diagnoses.
- In order to account for the health consequences of racism, clinicians should prioritize social history intake and be aware of how social and structural stressors perpetuate racial health inequities.
- We must adopt the same standards and guidelines for diagnosis and treatment of all patients regardless of race.
- Race cannot and should not be used as a biological determinant in clinical guidelines nor the research informing them. Rather, clinical guidelines on racial health outcomes must take into account the consequences of racism in racial health disparities. Racial differences are not the cause of disparities; they are the result of multilevel racism.
- Health-care providers play a key role in combating racism. In order to support their patients in feeling happy, healthy, and strong, clinicians must seek to affirm the strengths their patients bring, not assume they are a collection of risk factors. Clinicians need a paradigm shift to approaching patients of color as whole, rather than broken.
- Medicine must break down its own intellectual silos and hierarchy to build interdisciplinary alliances with thought leaders who have built foundations on the intersections of racism and health. Rather than using race as a differential diagnosis shortcut, elimination of race-based medicine presents an opportunity to call for interdisciplinary dialogue and action in solidarity with those from affected communities, critical race theorists, community-based organizations, and racial justice initiatives.
Next Steps
In order to move this vision forward, everyone from trainees to clinicians to critical race theorists to community members must not only read and dialogue, but also act. While barely scratching the surface, the following list offers a few suggestions to various types of readers to create and practice antiracist medicine.
Trainees
- Seek out literature and research on critical race theory and antiracist research. See appendix for suggestions.
- Teach yourself to question when you hear race used in clinical medicine.
- Ask questions of those around who are using race-based medicine. Question its usage, and teach others if you can.
- Don’t use race in the problem statement of your notes or clinical presentation.
- Seek out antiracist trainings in your area or online, especially if you are white or hold other privilege. This is for your patients, fellow trainees, and other providers.
- Organize for change. Push your educators to teach antiracist medicine and push for your clinicians to practice antiracist medicine. One idea:
- Don’t use the race-corrected GFR or spirometry values. Start a campaign to have your academic hospitals remove the race correction.
Clinicians and Providers
- Seek out literature and research on critical race theory and antiracist research. See appendix for suggestions.
- Seek out antiracist trainings in your area or online, especially if you are white or hold other privilege. This is for your patients, fellow providers, and staff.
- Teach yourself to question when you hear race used in clinical medicine.
- Use your power to ask questions of those around who are using race-based medicine. Question its usage, and teach others.
- Don’t use race in your notes or clinical presentation, especially not in the problem statement.
- Organize for change. Push yourself and your peers to teach and practice antiracist medicine. One idea:
- Don’t use the race-corrected GFR or spirometry values. Start a campaign to have your institution remove the race correction.
- Learn and use structural competency to begin to name and address the societal and structural factors that hinder patients’ ability to live to their highest level of well-being.
- Get active outside the clinic to address these structural issues.
- Help make medicine a less hostile space for both patients and providers.
Educators
- Seek out literature and research on critical race theory and antiracist research. See appendix for suggestions.
- Create a learning environment that is both safe for students and critical of race-based medicine. You must be trained in how to talk comfortably and critically about race in your classrooms and teaching settings. Seek out antiracist trainings to increase your skills and tools.
- Teach trainees in both critical race theory and the nuances of biology. Teach trainees to hold complexity and be powerful advocates for their patients.
Researchers
- Learn critical race theory and structural competency (see appendix for suggestions), and then use it to hold yourself to the highest precision in both research design and publishing. You cannot control what people will do afterward, but you can contribute to making a body of research that is rooted in antiracism and clearly spells out the implications of your findings.
- Seek out antiracist trainings in your area or online, especially if you are white or hold other privilege.
- Design and carry out research that corrects the current bad science. If the intended heuristic for using race in GFR is muscle mass, help find a marker of muscle mass or a faster way to measure it in clinic.
- Design and carry out research that measures and addresses root causes of poor health and health disparities, such as racism and structural causes.
Community-based Organizations
- Continue to form partnerships with physicians and clinics to address social and structural issues that impact well-being.
Community Members
- Question your provider’s use of race in your care. Some ideas (if you feel comfortable):
- Ask about the race correction factor if your clinician uses a measure like GFR or spirometry.
- Ask to see your patient record, and if race was used, ask your provider why it was relevant.
- Organize groups of patients to become patient-advocates, and get involved in the clinic’s patient advocacy board or other governing bodies.
Bibliography
Adow, Mohammed. “Nigeria’s Dangerous Skin Whitening Obsession.” Al Jazeera, April 6, 2013. https://www.aljazeera.com/indepth/features/2013/04/20134514845907984.ht….
Alberta Civil Liberties Research Centre. “Forms of Racism.” Accessed March 1, 2020. http://www.aclrc.com/forms-of-racism.
Alberta Civil Liberties Research Centre. “Racism and Power.” Accessed March 1, 2020. http://www.aclrc.com/racism-and-power.
Alexander, Michelle, and Cornel West. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York: The New Press, 2012.
Allen, Shauntice, Michelle V. Fanucchi, Lisa C. McCormick, and Kristina M. Zierold. “The Search for Environmental Justice: The Story of North Birmingham.” International Journal of Environmental Research and Public Health 16, no. 12 (June 14, 2019): 2117. https://doi.org/10.3390/ijerph16122117.
American Heart Association. “High Blood Pressure and African Americans.” October 31, 2016. https://www.heart.org/en/health-topics/high-blood-pressure/why-high-blo….
American Heart Association. “How High Blood Pressure Can Lead to Kidney Damage or Failure.” October 31, 2016. https://www.heart.org/en/health-topics/high-blood-pressure/health-threa….
American Psychological Association. “Featured Commentary: Trayvon, Troy, Sean: When Racial Biases and Microaggressions Kill.” July 2012. https://www.apa.org/pi/oema/resources/communique/2012/07/microaggressio….
Araujo, Andre B., Gretchen R. Chiu, Varant Kupelian, Susan A. Hall, Rachel E. Williams, Richard V. Clark, and John B. McKinlay. “Lean Mass, Muscle Strength, and Physical Function in a Diverse Population of Men: A Population-Based Cross-Sectional Study.” BMC Public Health 10, no. 1 (August 21, 2010): 508. https://doi.org/10.1186/1471-2458-10-508.
Bader, Eleanor J. “Racializing Lung Function.” Truthout. Accessed March 2, 2020. https://truthout.org/articles/racializing-lung-function/.
Bailey, Zinzi D., Nancy Krieger, Madina Agénor, Jasmine Graves, Natalia Linos, and Mary T. Bassett. “Structural Racism and Health Inequities in the USA: Evidence and Interventions.” The Lancet 389, no. 10077 (April 8, 2017): 1453–63. https://doi.org/10.1016/S0140-6736(17)30569-X.
Banks, Kira Hudson, and Jadah Stephens. “Reframing Internalized Racial Oppression and Charting a Way Forward.” Social Issues and Policy Review 12, no. 1 (2018): 91–111. https://doi.org/10.1111/sipr.12041.
Bhui, Professor Kamaldeep. “The Impact of Racism on Mental Health.” Synergi Collaborative Centre, March 2018.
Bivens, Donna. “Internalized Racism: A Definition.” Women’s Theological Center. 1995.
Black, Edwin. “Eugenics and the Nazis—the California Connection.” San Francisco Chronicle, November 9, 2003. https://www.sfgate.com/opinion/article/Eugenics-and-the-Nazis-the-Calif….
Braun, Lundy. Breathing Race into the Machine: The Surprising Career of the Spirometer from Plantation to Genetics. Minneapolis: University of Minnesota Press, 2014.
———. “Race, Ethnicity, and Health: Can Genetics Explain Disparities?” Perspectives in Biology and Medicine 45, no. 2 (May 1, 2002): 159–74. https://doi.org/10.1353/pbm.2002.0023.
———. “Race, Ethnicity and Lung Function: A Brief History.” Canadian Journal of Respiratory Therapy 51, no. 4 (2015): 99–101.
Bridges, Khiara M. Reproducing Race: An Ethnography of Pregnancy as a Site of Racialization. Berkeley: University of California Press, 2011.
Brody, Gene H., Man-Kit Lei, David H. Chae, Tianyi Yu, Steven M. Kogan, and Steven R. H. Beach. “Perceived Discrimination among African American Adolescents and Allostatic Load: A Longitudinal Analysis with Buffering Effects.” Child Development 85, no. 3 (May 2014): 989–1002. https://doi.org/10.1111/cdev.12213.
Brown, S. A., A. A. Garcia, K. Kouzekanani, and C. L. Hanis. “Culturally Competent Diabetes Self-Management Education for Mexican Americans: The Starr County Border Health Initiative.” Diabetes Care 25, no. 2 (February 1, 2002): 259–68. https://doi.org/10.2337/diacare.25.2.259.
Centers for Disease Control and Prevention. “Social Determinants of Health.” April 9, 2019. https://www.cdc.gov/socialdeterminants/index.htm
Chambers, Earle C., Eugene S. Tull, Henry S. Fraser, Nyasha R. Mutunhu, Natasha Sobers, and Elisa Niles. “The Relationship of Internalized Racism to Body Fat Distribution and Insulin Resistance among African Adolescent Youth.” Journal of the National Medical Association 96, no. 12 (December 2004): 1594–98.
Chen, Wei-Liang, Chung-Ching Wang, Li-Wei Wu, Tung-Wei Kao, James Yi-Hsin Chan, Ying-Jen Chen, Ya-Hui Yang, Yaw-Wen Chang, and Tao-Chun Peng. “Relationship between Lung Function and Metabolic Syndrome.” PLoS ONE 9, no. 10 (October 9, 2014). https://doi.org/10.1371/journal.pone.0108989.
Chou, Vivian. “How Science and Genetics Are Reshaping the Race Debate of the 21st Century.” Science in the News (blog), April 17, 2017. http://sitn.hms.harvard.edu/flash/2017/science-genetics-reshaping-race-….
Cohn, S. H., C. Abesamis, I. Zanzi, J. F. Aloia, S. Yasumura, and K. J. Ellis. “Body Elemental Composition: Comparison between Black and White Adults.” The American Journal of Physiology 232, no. 4 (April 1977): E419-422. https://doi.org/10.1152/ajpendo.1977.232.4.E419.
Crear-Perry, Joia. “Root Causes of Black Maternal Health Inequities. Improving Access to Perinatal Care: Confronting Disparities & Inequities in Maternal-Infant Health.” National Birth Equity Collaborative, April 2019, 50.
Crenshaw, Kimberle. “Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color.” Stanford Law Review 43, no. 6 (1991): 1241–99. https://doi.org/10.2307/1229039.
Critical Resistance. “What Is the PIC? What Is Abolition?” Accessed March 3, 2020. http://criticalresistance.org/about/not-so-common-language/.
Culver, Bruce H., Brian L. Graham, Allan L. Coates, Jack Wanger, Cristine E. Berry, Patricia K. Clarke, Teal S. Hallstrand, et al. “Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement.” American Journal of Respiratory and Critical Care Medicine 196, no. 11 (December 2017): 1463–72. https://doi.org/10.1164/rccm.201710-1981ST.
Cutler, David M., Roland G. Fryer, and Edward L. Glaeser. “Racial Differences in Life Expectancy: The Impact of Salt, Slavery, and Selection.” Unpublished manuscript, Harvard University and the National Bureau of Economic Research, March 1, 2005.
Digitale, Erin. “Microaggressions in Medical Training: Understanding, and Addressing, the Problem.” Scope (blog), May 22, 2018. https://scopeblog.stanford.edu/2018/05/22/185969/.
Drake, Katherine A., Joshua M. Galanter, and Esteban Gonzalez Burchard. “Race, Ethnicity and Social Class and the Complex Etiologies of Asthma.” Pharmacogenomics 9, no. 4 (April 2008): 453–62. https://doi.org/10.2217/14622416.9.4.453.
Dubner, Stephen J. “Toward a Unified Theory of Black America.” New York Times, March 20, 2005, sec. Magazine. https://www.nytimes.com/2005/03/20/magazine/toward-a-unified-theory-of-….
Duong, MyLinh, Shofiqul Islam, Sumathy Rangarajan, Koon Teo, Paul M. O’Byrne, Holger J. Schünemann, Ehimario Igumbor, et al. “Global Differences in Lung Function by Region (PURE): An International, Community-Based Prospective Study.” The Lancet Respiratory Medicine 1, no. 8 (October 1, 2013): 599–609. https://doi.org/10.1016/S2213-2600(13)70164-4.
Duster, Troy. “Buried Alive.” In Genetic Nature/Culture: Anthropology and Science beyond the Two-Culture Divide, edited by Alan H. Goodman, Deborah Heath, and M. Susan Lindee, 258–77. University of California Press, 2003. www.jstor.org/stable/10.1525/j.ctt1pp2bv.19.
———. “Race and Reification in Science.” Science 307, no. 5712 (February 18, 2005): 1050–51. https://doi.org/10.1126/science.1110303.
Edwards, Robert R. “The Association of Perceived Discrimination with Low Back Pain.” Journal of Behavioral Medicine 31, no. 5 (October 2008): 379–89. https://doi.org/10.1007/s10865-008-9160-9.
Fausto-Sterling, Anne. “I Can’t Breathe.” Boston Review, March 17, 2016. http://bostonreview.net/wonders/anne-fausto-sterling-race-medical-school.
Francis, Darlene D. “Conceptualizing Child Health Disparities: A Role for Developmental Neurogenomics.” Pediatrics 124, no. 3 (November 2009): S196–202. https://doi.org/10.1542/peds.2009-1100G.
Fullwiley, Duana. “The Biologistical Construction of Race: ‘Admixture’ Technology and the New Genetic Medicine.” Social Studies of Science 38, no. 5 (October 1, 2008): 695–735. https://doi.org/10.1177/0306312708090796.
Gellene, Denise. “Heart Pill Intended Only for Blacks Sparks Debate.” Los Angeles Times, June 16, 2005.
Gould, Stephen Jay. The Mismeasure of Man. W. W. Norton & Company, 1996.
Gravlee, Clarence C. “How Race Becomes Biology: Embodiment of Social Inequality.” American Journal of Physical Anthropology 139, no. 1 (May 1, 2009): 47–57. https://doi.org/10.1002/ajpa.20983.
———. “How Race Becomes Biology: Embodiment of Social Inequality.” American Journal of Physical Anthropology 139, no. 1 (May 1, 2009): 47–57. https://doi.org/10.1002/ajpa.20983.
Hällgren, Camilla, and Gaby Weiner. “Out of the Shadow of Linnaeus: Acknowledging Their Existence and Seeking to Challenge, Racist Practices in Swedish Educational Settings,” 2006. http://www.leeds.ac.uk/educol/documents/157423.htm.
Hankinson, John L., John R. Odencrantz, and Kathleen B. Fedan. “Spirometric Reference Values from a Sample of the General US Population.” American Journal of Respiratory and Critical Care Medicine 159, no. 1 (January 1, 1999): 179–87. https://doi.org/10.1164/ajrccm.159.1.9712108.
———. “Spirometric Reference Values from a Sample of the General US Population.” American Journal of Respiratory and Critical Care Medicine 159, no. 1 (January 1, 1999): 179–87. https://doi.org/10.1164/ajrccm.159.1.9712108.
Harsha, David W., Ralph R. Frerichs, and Gerald S. Berenson. “Densitometry and Anthropometry of Black and White Children.” Human Biology 50, no. 3 (1978): 261–80.
Hawkins, B. The New Plantation: Black Athletes, College Sports, and Predominantly White NCAA Institutions. Palgrave Macmillan US, 2010. https://doi.org/10.1057/9780230105539.
“High Blood Pressure in African-Americans: Genetics, Risks, Causes, and More.” WebMD. Accessed March 1, 2020. https://www.webmd.com/hypertension-high-blood-pressure/guide/hypertensi….
Hipolito-Delgado, Carlos P. “Exploring the Etiology of Ethnic Self-Hatred: Internalized Racism in Chicana/o and Latina/o College Students.” Journal of College Student Development 51, no. 3 (May 23, 2010): 319–31. https://doi.org/10.1353/csd.0.0133.
Hoffman, Kelly M., Sophie Trawalter, Jordan R. Axt, and M. Norman Oliver. “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences between Blacks and Whites.” Proceedings of the National Academy of Sciences 113, no. 16 (April 19, 2016): 4296–4301. https://doi.org/10.1073/pnas.1516047113.
Holmes, Ian. “David Reich, Racism, and the Difficulty of Talking About Genetics.” The Atlantic, April 25, 2018. https://www.theatlantic.com/science/archive/2018/04/reich-genetics-raci….
James, Paul A., Suzanne Oparil, Barry L. Carter, William C. Cushman, Cheryl Dennison-Himmelfarb, Joel Handler, Daniel T. Lackland, et al. “2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee.” Journal of the American Medical Association 311, no. 5 (February 5, 2014): 507–20. https://doi.org/10.1001/jama.2013.284427.
John-Henderson, Neha A., Jennifer E. Stellar, Rodolfo Mendoza-Denton, and Darlene D. Francis. “Socioeconomic Status and Social Support: Social Support Reduces Inflammatory Reactivity for Individuals Whose Early-Life Socioeconomic Status Was Low.” Psychological Science 26, no. 10 (October 1, 2015): 1620–29. https://doi.org/10.1177/0956797615595962.
Johnson, Alexis McGill, Rachel D. Godsil, and Isaac Butler. “The Science of Equality, Volume 1: Addressing Implicit Bias, Racial Anxiety, and Stereotype Threat in Education and Healthcare.” Perception Institute 1 (November 2014): 90.
Johnston-Goodstar, Katie, and Ross VeLure Roholt. “‘Our Kids Aren’t Dropping Out; They’re Being Pushed Out’: Native American Students and Racial Microaggressions in Schools.” Journal of Ethnic & Cultural Diversity in Social Work 26, no. 1–2 (January 2, 2017): 30–47. https://doi.org/10.1080/15313204.2016.1263818.
Juster, Robert-Paul, Jennifer J. Russell, Daniel Almeida, and Martin Picard. “Allostatic Load and Comorbidities: A Mitochondrial, Epigenetic, and Evolutionary Perspective.” Development and Psychopathology 28, no. 4pt1 (2016): 1117–46. https://doi.org/10.1017/S0954579416000730.
Kahn, Jonathan. “From Disparity to Difference: How Race-Specific Medicines May Undermine Policies to Address Inequalities in Health Care.” Southern California Interdisciplinary Law Journal 15, no. 1 (2005): 105–30.
Katzung, Bertram. Basic and Clinical Pharmacology, 14th edition. New York: McGraw-Hill Education/Medical, 2017.
Kiefer, Elizabeth M., John L. Hankinson, and R. Graham Barr. “Similar Relation of Age and Height to Lung Function Among Whites, African Americans, and Hispanics.” American Journal of Epidemiology 173, no. 4 (February 15, 2011): 376–87. https://doi.org/10.1093/aje/kwq417.
Kramar, David E., Aaron Anderson, Hayley Hilfer, Karen Branden, and John J. Gutrich. “A Spatially Informed Analysis of Environmental Justice: Analyzing the Effects of Gerrymandering and the Proximity of Minority Populations to US Superfund Sites.” Environmental Justice 11, no. 1 (February 2018): 29–39. https://doi.org/10.1089/env.2017.0031.
Kumar, Rajesh, Max A. Seibold, Melinda C. Aldrich, L. Keoki Williams, Alex P. Reiner, Laura Colangelo, Joshua Galanter, et al. “Genetic Ancestry in Lung-Function Predictions.” New England Journal of Medicine 363, no. 4 (July 22, 2010): 321–30. https://doi.org/10.1056/NEJMoa0907897.
Kumar, Vinay, Abul K. Abbas, and Jon C. Aster. Robbins and Cotran Pathologic Basis of Disease, 9th edition. Philadelphia, PA: Elsevier, 2014.
Kuzawa, Christopher W., and Elizabeth Sweet. “Epigenetics and the Embodiment of Race: Developmental Origins of US Racial Disparities in Cardiovascular Health.” American Journal of Human Biology 21, no. 1 (2009): 2–15. https://doi.org/10.1002/ajhb.20822.
Levey, A. S., J. P. Bosch, J. B. Lewis, T. Greene, N. Rogers, and D. Roth. “A More Accurate Method to Estimate Glomerular Filtration Rate from Serum Creatinine: A New Prediction Equation. Modification of Diet in Renal Disease Study Group.” Annals of Internal Medicine 130, no. 6 (March 16, 1999): 461–70. https://doi.org/10.7326/0003-4819-130-6-199903160-00002.
Levey, Andrew S., Lesley A. Stevens, Christopher H. Schmid, Yaping Lucy Zhang, Alejandro F. Castro, Harold I. Feldman, John W. Kusek, et al. “A New Equation to Estimate Glomerular Filtration Rate.” Annals of Internal Medicine 150, no. 9 (May 5, 2009): 604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Lewis, Tené T., Susan A. Everson-Rose, Lynda H. Powell, Karen A. Matthews, Charlotte Brown, Kelly Karavolos, Kim Sutton-Tyrrell, Elizabeth Jacobs, and Deidre Wesley. “Chronic Exposure to Everyday Discrimination and Coronary Artery Calcification in African-American Women: The SWAN Heart Study.” Psychosomatic Medicine 68, no. 3 (June 2006): 362–368. https://doi.org/10.1097/01.psy.0000221360.94700.16.
Li, Eric P. H., Hyun Jeong Min, and Russell W. Belk. “Skin Lightening and Beauty in Four Asian Cultures.” Association for Consumer Research, North American Advances 35 (2008). https:///www.acrwebsite.org/volumes/13415/volumes/v35/NA-35.
Lipson, Juliene G., and Suzanne L. Dibble, eds. Culture & Nursing Care: A Pocket Guide. San Francisco: University of California, San Francisco, Nursing Press, 1996.
Lipson, Juliene G., and Suzanne L. Dibble, eds. Culture & Clinical Care. San Francisco, CA: University of California, San Francisco, Nursing Press, 2005.
Lujan, Heidi L., and Stephen E. DiCarlo. “The ‘African Gene’ Theory: It Is Time to Stop Teaching and Promoting the Slavery Hypertension Hypothesis.” Advances in Physiology Education 42, no. 3 (July 4, 2018): 412–16. https://doi.org/10.1152/advan.00070.2018.
Lukachko, Alicia, Mark L. Hatzenbuehler, and Katherine M. Keyes. “Structural Racism and Myocardial Infarction in the United States.” Social Science & Medicine 103 (February 2014): 42–50. https://doi.org/10.1016/j.socscimed.2013.07.021.
M, A &. “Internalized Racism Among Asians.” Medium, October 14, 2018. https://medium.com/a-m-awaken-your-inner-asian/internalized-racism-amon….
Martin, Toni. “The Color of Kidneys.” American Journal of Kidney Diseases 58, no. 5 (November 1, 2011): A27–28. https://doi.org/10.1053/j.ajkd.2011.08.018.
Maurer, Frances A., and Claudia M. Smith, eds. Community/Public Health Nursing Practice: Health for Families and Populations, 5th ed. St. Louis, Mo: Elsevier/Saunders, 2013.
McGeachie, Michael J., George L. Clemmer, Damien C. Croteau‐Chonka, Peter J. Castaldi, Michael H. Cho, Joanne E. Sordillo, Jessica A. Lasky‐Su, Benjamin A. Raby, Kelan G. Tantisira, and Scott T. Weiss. “Whole Genome Prediction and Heritability of Childhood Asthma Phenotypes.” Immunity, Inflammation and Disease 4, no. 4 (November 28, 2016): 487–96. https://doi.org/10.1002/iid3.133.
Mendoza, Roger Lee. “The Skin Whitening Industry in the Philippines.” Journal of Public Health Policy 35, no. 2 (May 1, 2014): 219–38. https://doi.org/10.1057/jphp.2013.50.
Menezes, Ana Maria B., Fernando C. Wehrmeister, Fernando P. Hartwig, Rogelio Perez-Padilla, Denise P. Gigante, Fernando C. Barros, Isabel O. Oliveira, Gustavo D. Ferreira, and Bernardo L. Horta. “African Ancestry, Lung Function and the Effect of Genetics.” The European Respiratory Journal 45, no. 6 (June 2015): 1582–89. https://doi.org/10.1183/09031936.00112114.
Meredith C. McCormack. “Selecting Reference Values for Pulmonary Function Tests.” UpToDate, July 24, 2018. https://www-uptodate-com.ucsf.idm.oclc.org/contents/selecting-reference….
Psychology Today. “Microaggressions: More Than Just Race.” Accessed March 1, 2020. http://www.psychologytoday.com/blog/microaggressions-in-everyday-life/2….
Moraga, Cherríe, and Gloria Anzaldúa, eds. This Bridge Called My Back: Writings by Radical Women of Color, 4th edition. Albany: State University of New York Press, 2015.
Nadal, Kevin L., Katie E. Griffin, Yinglee Wong, Kristin C. Davidoff, and Lindsey S. Davis. “The Injurious Relationship Between Racial Microaggressions and Physical Health: Implications for Social Work.” Journal of Ethnic & Cultural Diversity in Social Work 26, no. 1–2 (January 2, 2017): 6–17. https://doi.org/10.1080/15313204.2016.1263813.
Nadal, Kevin L., Katie E. Griffin, Yinglee Wong, Sahran Hamit, and Morgan Rasmus. “The Impact of Racial Microaggressions on Mental Health: Counseling Implications for Clients of Color.” Journal of Counseling & Development 92, no. 1 (2014): 57–66. https://doi.org/10.1002/j.1556-6676.2014.00130.x.
Nardone, Anthony, Joan A. Casey, Rachel Morello-Frosch, Mahasin Mujahid, John R. Balmes, and Neeta Thakur. “Associations between Historical Residential Redlining and Current Age-Adjusted Rates of Emergency Department Visits Due to Asthma across Eight Cities in California: An Ecological Study.” The Lancet Planetary Health 4, no. 1 (January 1, 2020): e24–31. https://doi.org/10.1016/S2542-5196(19)30241-4.
National Kidney Foundation. “Frequently Asked Questions about GFR Estimates.” 2014. https://www.kidney.org/sites/default/files/docs/12-10-4004_abe_faqs_abo…
Nicholas, Susanne B., Kamyar Kalantar-Zadeh, and Keith C. Norris. “Racial Disparities in Kidney Disease Outcomes.” Seminars in Nephrology 33, no. 5 (September 2013): 409–15. https://doi.org/10.1016/j.semnephrol.2013.07.002.
Norton, Jenna M., Marva M. Moxey-Mims, Paul W. Eggers, Andrew S. Narva, Robert A. Star, Paul L. Kimmel, and Griffin P. Rodgers. “Social Determinants of Racial Disparities in CKD.” Journal of the American Society of Nephrology 27, no. 9 (September 2016): 2576–95. https://doi.org/10.1681/ASN.2016010027.
Nuru-Jeter, Amani, David H. Chae, Melisa Price, James Telesford, Rodolfo Mendoza-Denton, and Cheryl Woods-Giscombe. “Abstract 9550: Anticipatory Racism Threat and Superwoman Schema: Elucidating the Relationship Between Racial Discrimination and Chronic Inflammation.” Circulation 128, no. 22 (November 26, 2013): A9550–A9550. https://www.ahajournals.org/doi/abs/10.1161/circ.128.suppl_22.a9550.
Obasogie, Osagie K. “The Return of Biological Race? Regulating Race and Genetics Through Administrative Agency Race Impact Assessments.” Southern California Indterdisciplinary Law Jounral 22 (January 1, 2012): 1.
Obasogie, Osagie K. “Oprah’s Unhealthy Mistake.” Los Angeles Times, May 17, 2007. https://www.latimes.com/archives/la-xpm-2007-may-17-oe-obasogie17-story….
Omi, Michael, and Howard Winant. Racial Formation in the United States. Routledge, 2014.
O’Neill Hayes, Tara, and Carly McNeil. “Maternal Mortality in the United States.” American Action Forum, September 9, 2019. https://www.americanactionforum.org/insight/maternal-mortality-in-the-u….
Orgera, Kendal, and Artiga, Samantha. “Disparities in Health and Health Care: Five Key Questions and Answers.” The Henry J. Kaiser Family Foundation (blog), August 8, 2018. https://www.kff.org/disparities-policy/issue-brief/disparities-in-healt….
Parker, Margaret M., Marilyn G. Foreman, Haley J. Abel, Rasika A. Mathias, Jacqueline B. Hetmanski, James D. Crapo, Edwin K. Silverman, Terri H. Beaty, and the COPDGene Investigators. “Admixture Mapping Identifies a Quantitative Trait Locus Associated with FEV1/FVC in the COPDGene Study.” Genetic Epidemiology 38, no. 7 (November 2014): 652–59. https://doi.org/10.1002/gepi.21847.
Pellegrino, R., G. Viegi, V. Brusasco, R. O. Crapo, F. Burgos, R. Casaburi, A. Coates, et al. “Interpretative Strategies for Lung Function Tests.” The European Respiratory Journal 26, no. 5 (November 2005): 948–68. https://doi.org/10.1183/09031936.05.00035205.
Peralta, Carmen A., Feng Lin, Michael G. Shlipak, David Siscovick, Cora Lewis, David R. Jacobs, and Kirsten Bibbins-Domingo. “Race Differences in Prevalence of Chronic Kidney Disease among Young Adults Using Creatinine-Based Glomerular Filtration Rate-Estimating Equations.” Nephrology Dialysis Transplantation 25, no. 12 (December 2010): 3934–39. https://doi.org/10.1093/ndt/gfq299.
Phelan, Jo C., Bruce G. Link, and Parisa Tehranifar. “Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications.” Journal of Health and Social Behavior 51, no. 1 (March 2010): S28–40. https://doi.org/10.1177/0022146510383498.
Quanjer, Philip H., Sanja Stanojevic, Tim J. Cole, Xaver Baur, Graham L. Hall, Bruce H. Culver, Paul L. Enright, et al. “Multi-Ethnic Reference Values for Spirometry for the 3–95 Year Age Range: The Global Lung Function 2012 Equations.” The European Respiratory Journal 40, no. 6 (December 2012): 1324–43. https://doi.org/10.1183/09031936.00080312.
Reichel, Chloe. “Toxic Waste Sites and Environmental Justice: Research Roundup.” Journalist’s Resource (blog), September 24, 2018. https://journalistsresource.org/studies/environment/superfund-toxic-was….
Remnick, David. “Ten Years After ‘The New Jim Crow.’” The New Yorker, January 17, 2020. https://www.newyorker.com/news/the-new-yorker-interview/ten-years-after….
Richman, Laura Smart, and Charles Jonassaint. “The Effects of Race-Related Stress on Cortisol Reactivity in the Laboratory: Implications of the Duke Lacrosse Scandal.” Annals of Behavioral Medicine 35, no. 1 (February 1, 2008): 105–10. https://doi.org/10.1007/s12160-007-9013-8.
Ripp, Kelsey, and Lundy Braun. “Race/Ethnicity in Medical Education: An Analysis of a Question Bank for Step 1 of the United States Medical Licensing Examination.” Teaching and Learning in Medicine 29, no. 2 (June 2017): 115–22. https://doi.org/10.1080/10401334.2016.1268056.
Roberts, Dorothy E. “The Problem with Race-Based Medicine,” TEDMED talk (video). 2015. https://www.ted.com/talks/dorothy_roberts_the_problem_with_race_based_m….
———. “What’s Wrong with Race-Based Medicine?” Faculty Scholarship at Penn Law, January 1, 2011. https://scholarship.law.upenn.edu/faculty_scholarship/435.
———. “Constructing a Criminal Justice System Free of Racial Bias: An Abolitionist Framework.” Columbia Human Rights Law Review 261 (2008).
———. “Is Race-Based Medicine Good for Us?: African American Approaches to Race, Biomedicine, and Equality” The Journal of Law, Medicine & Ethics (August 1, 2008). http://journals.sagepub.com/doi/10.1111/j.1748-720X.2008.302.x.
———. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York: Vintage Books, 2014. http://rbdigital.oneclickdigital.com.
US News & World Report. “Rub Out the Bias Behind Skin-Lightening Products.” Accessed March 3, 2020. https://www.usnews.com/news/best-countries/articles/2017-04-17/global-w….
Sawyer, Pamela J., Brenda Major, Bettina J. Casad, Sarah S. M. Townsend, and Wendy Berry Mendes. “Discrimination and the Stress Response: Psychological and Physiological Consequences of Anticipating Prejudice in Interethnic Interactions.” American Journal of Public Health 102, no. 5 (March 15, 2012): 1020–26. https://doi.org/10.2105/AJPH.2011.300620.
Sedrak, Aziza, and Noah Kondamudi. “Sickle Cell Disease.” StatPearls, November 18, 2019. https://www.statpearls.com/kb/viewarticle/29015.
Shaban, Hamza. “How Racism Creeps Into Medicine.” The Atlantic, August 29, 2014. https://www.theatlantic.com/health/archive/2014/08/how-racism-creeps-in….
Silva, Analiza M., Wei Shen, Moonseong Heo, Dympna Gallagher, Zimian Wang, Luis B. Sardinha, and Steven B. Heymsfield. “Ethnicity-Related Skeletal Muscle Differences across the Lifespan.” American Journal of Human Biology 22, no. 1 (February 2010): 76–82. https://doi.org/10.1002/ajhb.20956.
Sims, Mario, Ana V. Diez-Roux, Amanda Dudley, Samson Gebreab, Sharon B. Wyatt, Marino A. Bruce, Sherman A. James, Jennifer C. Robinson, David R. Williams, and Herman A. Taylor. “Perceived Discrimination and Hypertension Among African Americans in the Jackson Heart Study.” American Journal of Public Health 102, no. 2 (May 2012): S258–65. https://doi.org/10.2105/AJPH.2011.300523.
Smith, Andrea. “Heteropatriarchy and the Three Pillars of White Supremacy: Rethinking Women of Color Organizing.” In Color of Violence, edited by INCITE! Women of Color Against Violence, 66–73. Duke University Press, 2016. https://doi.org/10.1215/9780822373445-007.
Stanhope, Marcia, and Jeanette Lancaster. Public Health Nursing: Population-Centered Health Care in the Community. London: Elsevier Health Sciences, 2014. http://public.ebookcentral.proquest.com/choice/publicfullrecord.aspx?p=….
Sue, Derald Wing, Christina M. Capodilupo, Gina C. Torino, Jennifer M. Bucceri, Aisha M. B. Holder, Kevin L. Nadal, and Marta Esquilin. “Racial Microaggressions in Everyday Life: Implications for Clinical Practice.” American Psychologist 62, no. 4 (2007): 271–86. https://doi.org/10.1037/0003-066X.62.4.271.
Sullivan, Shannon. “Inheriting Racist Disparities in Health: Epigenetics and the Transgenerational Effects of White Racism.” Critical Philosophy of Race 1, no. 2 (September 5, 2013): 190–218.
Svetaz, Maria Veronica, Veenod Chulani, Kimberly J. West, Raina Voss, Michele A. Kelley, Marissa Raymond-Flexch, Wanda Thruston, Tamera Coyne-Beasley, Melissa Kang, and Enoch Leung. “Racism and Its Harmful Effects on Nondominant Racial–Ethnic Youth and Youth-Serving Providers: A Call to Action for Organizational Change: The Society for Adolescent Health and Medicine.” Journal of Adolescent Health 63, no. 2 (August 1, 2018): 257–61. https://doi.org/10.1016/j.jadohealth.2018.06.003.
Taylor, Teletia R., Carla D. Williams, Kepher H. Makambi, Charles Mouton, Jules P. Harrell, Yvette Cozier, Julie R. Palmer, Lynn Rosenberg, and Lucile L. Adams-Campbell. “Racial Discrimination and Breast Cancer Incidence in US Black Women: The Black Women’s Health Study.” American Journal of Epidemiology 166, no. 1 (July 1, 2007): 46–54. https://doi.org/10.1093/aje/kwm056.
Taylor, Telford. “Trials of War Criminals before the Nuernberg Military Tribunals under Control Council Law No. 10,” Military Legal Resource (n.d.).
Tervalon, Melanie, and Jann Murray-García. “Cultural Humility versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” Journal of Health Care for the Poor and Underserved 9, no. 2 (1998): 117–25. https://doi.org/10.1353/hpu.2010.0233.
Texeira, Erin. “Racial Basis for Asbestos Lawsuits?; Owens Corning Seeks More Stringent Standards for Blacks.” Baltimore Sun, March 25, 1999. https://www.baltimoresun.com/news/bs-xpm-1999-03-25-9903250041-story.ht….
The American College of Obstetricians and Gynecologists (@ACOGAction). “The answer is...B. #ACOG19 Bipolar disorder increases risk of suicide.” Twitter, May 4, 2019. https://twitter.com/acogaction/status/1124713954977165312.
The Aspen Institute: Roundtable on Community Change. “Glossary for Understanding the Dismantling Structural Racism/Promoting Racial Equity Analysis.” Accessed March 1, 2020. https://assets.aspeninstitute.org/content/uploads/files/content/docs/rc….
Thomas, David Hurst, and Vine Deloria Jr. Skull Wars: Kennewick Man, Archaeology, and the Battle for Native American Identity. New York: Basic Books, 2001.
Torres, Lucas, Mark W. Driscoll, and Anthony L. Burrow. “Racial Microaggressions and Psychological Functioning Among Highly Achieving African-Americans: A Mixed-Methods Approach.” Journal of Social and Clinical Psychology 29, no. 10 (December 1, 2010): 1074–99. https://doi.org/10.1521/jscp.2010.29.10.1074.
Troxel, Wendy M., Karen A. Matthews, Joyce T. Bromberger, and Kim Sutton-Tyrrell. “Chronic Stress Burden, Discrimination, and Subclinical Carotid Artery Disease in African American and Caucasian Women.” Health Psychology 22, no. 3 (2003): 300–309. https://doi.org/10.1037/0278-6133.22.3.300.
Tull, S. E., T. Wickramasuriya, J. Taylor, V. Smith-Burns, M. Brown, G. Champagnie, K. Daye, et al. “Relationship of Internalized Racism to Abdominal Obesity and Blood Pressure in Afro-Caribbean Women.” Journal of the National Medical Association 91, no. 8 (August 1999): 447–52.
Wagner, D. R., and V. H. Heyward. “Measures of Body Composition in Blacks and Whites: A Comparative Review.” The American Journal of Clinical Nutrition 71, no. 6 (June 2000): 1392–1402. https://doi.org/10.1093/ajcn/71.6.1392.
Wallack, Lawrence, and Kent Thornburg. “Developmental Origins, Epigenetics, and Equity: Moving Upstream.” Maternal and Child Health Journal 20, no. 5 (May 1, 2016): 935–40. https://doi.org/10.1007/s10995-016-1970-8.
Walls, M. L., J. Gonzalez, T. Gladney, and E. Onello. “Unconscious Biases: Racial Microaggressions in American Indian Health Care.” The Journal of the American Board of Family Medicine 28, no. 2 (March 1, 2015): 231–39. https://doi.org/10.3122/jabfm.2015.02.140194.
Watts‐Jones, Dee. “Healing Internalized Racism: The Role of a Within-Group Sanctuary Among People of African Descent.” Family Process 41, no. 4 (2002): 591–601. https://doi.org/10.1111/j.1545-5300.2002.00591.x.
University of California, Los Angeles, School of Public Affairs. “What Is Critical Race Theory?” November 4, 2009. https://spacrs.wordpress.com/what-is-critical-race-theory/.
White, Ben. “How to Approach NBME/USMLE Questions.” July 21, 2013. https://www.benwhite.com/medicine/how-to-approach-nbme-usmle-questions/.
Wilkinson, Emma, Alison Brettle, Muhammad Waqar, and Gurch Randhawa. “Inequalities and Outcomes: End Stage Kidney Disease in Ethnic Minorities.” BMC Nephrology 20, no. 1 (June 26, 2019): 234. https://doi.org/10.1186/s12882-019-1410-2.
Williams, David R., and Selina A. Mohammed. “Racism and Health I: Pathways and Scientific Evidence.” The American Behavioral Scientist 57, no. 8 (August 1, 2013). https://doi.org/10.1177/0002764213487340.
Williams, Stephen K., Joseph Ravenell, Sara Seyedali, Sam Nayef, and Gbenga Ogedegbe. “Hypertension Treatment in Blacks: Discussion of the US Clinical Practice Guidelines.” Progress in Cardiovascular Diseases 59, no. 3 (2016): 282–88. https://doi.org/10.1016/j.pcad.2016.09.004.
Worrall, J. G., V. Phongsathorn, R. J. Hooper, and E. W. Paice. “Racial Variation in Serum Creatine Kinase Unrelated to Lean Body Mass.” British Journal of Rheumatology 29, no. 5 (October 1990): 371–73. https://doi.org/10.1093/rheumatology/29.5.371.
Yudell, Michael, Dorothy Roberts, Rob DeSalle, and Sarah Tishkoff. “Taking Race out of Human Genetics.” Science 351, no. 6273 (February 5, 2016): 564–65. https://doi.org/10.1126/science.aac4951.
Zanocco, Juliana A., Sonia K. Nishida, Michelle Tiveron Passos, Amélia Rodrigues Pereira, Marcelo S. Silva, Aparecido B. Pereira, and Gianna Mastroianni Kirsztajn. “Race Adjustment for Estimating Glomerular Filtration Rate Is Not Always Necessary.” Nephron Extra 2, no. 1 (January 2012): 293–302. https://doi.org/10.1159/000343899.
Zeh, Peter, Ann-Marie Cannaby, Harbinder K. Sandhu, Jane Warwick, and Jackie A. Sturt. “A Cross-Sectional Survey of General Practice Health Workers’ Perceptions of Their Provision of Culturally Competent Services to Ethnic Minority People with Diabetes.” Primary Care Diabetes 12, no. 6 (December 1, 2018): 501–9. https://doi.org/10.1016/j.pcd.2018.07.016.
Appendix: For Further Reading
The following is a partial, imperfect, ever-in-progress list of scholars and works we have found useful. This is neither the beginning nor the end of the conversation, but squarely in the middle. As build the changes we need, we are grateful for the foundational work of these scholars and activists.
Womxn of Color Scholars on Race and Medicine
-
Dorothy Roberts, Fatal Invention and Killing the Black Body
-
Kimberley Crenshaw
-
Joia Crear-Perry
-
Khiara Bridges
-
Tina Sacks
-
INCITE!
-
Melanie Tervalon and Jann Murray-Garcia “Cultural Humility versus Cultural Competence” (1998)
Racism, Not Race, Causes Health Disparities
-
The Urban Institute and the Virginia Commonwealth University’s Center on Society and Health briefs on income and health: https://www.urban.org/sites/default/files/publication/49116/2000178-How-are-Income-and-Wealth-Linked-to-Health-and-Longevity.pdf
-
Link and Phelan, “Social Conditions as Fundamental Causes of Disease” (1995): https://www.jstor.org/stable/2626958?seq=1
-
Phelan and Link, “Social Conditions as Fundamental Causes of Health Inequalities” (2010): https://doi.org/10.1177/0022146510383498
-
Clarence Gravlee, “How Race Becomes Biology: Embodiment of Social Inequality” (2009) (and other later works): https://doi.org/10.1002/ajpa.20983
-
Thomas A. LaVeist, “Disentangling Race and Socioeconomic Status: A Key to Understanding Health Inequalities” (2005): https://doi.org/10.1093/jurban/jti061
White Supremacy Dismantling
-
Layla F. Saad, Me and White Supremacy workbook: https://www.meandwhitesupremacybook.com/
-
White Noise Collective: https://www.conspireforchange.org/resources/
-
Resources from INCITE!: https://incite-national.org/2019/07/31/new-resources-for-transformative-justice-and-community-accountability/
-
University of California, San Francisco, OB-GYN Grand Rounds talk on White Fragility (12/10/19): https://obgyn.ucsf.edu/education-training/grand-rounds
-
Teaching resources from the 2006 Stop Dreaming, Keep Working Workshop: https://www.lsu.edu/hss/wgs/files/nwsateachingraceguide.pdf
-
Tim Wise books and DVDs: http://www.timwise.org/books-and-dvds/
Fundamental Texts and Resources in Race-Based Medicine
-
Dorothy Roberts, “The Problem with Race-Based Medicine,” TEDMED (2015): https://www.ted.com/talks/dorothy_roberts_the_problem_with_race_based_medicine/transcript?language=en
-
Dorothy Roberts, “What’s Wrong with Race-Based Medicine?” (2011)
-
Janet K. Shim, Heart-Sick: The Politics of Risk, Inequality, and Heart Disease (2014)
- 7These quotes are kept anonymous to prevent readers from within our medical school communities to specifically identify who the stories are about.
- 8Kendal Orgera and Samantha Artiga, “Disparities in Health and Health Care,” The Henry J. Kaiser Family Foundation (blog) (August 8, 2018).
- 9Paula Braveman, “What Are Health Disparities and Health Equity? We Need to Be Clear,” Public Health Reports (Washington, DC: 1974), 129, no. 2 (2014): 5–8. doi:10.1177/00333549141291S203.
- 10Clarence C. Gravlee, “How Race Becomes Biology: Embodiment of Social Inequality,” American Journal of Physical Anthropology 139, no. 1 (May 1, 2009): 47–57. https://doi.org/10.1002/ajpa.20983.
- 11Graphic adapted by Dr. Joia Crear-Perry, who adapted it from MPHI from Richard Hofrichter and Rajiv Bhatia, Tackling Health Inequities through Public Health Practice (New York: Oxford University Press, 2010).
- 12Joia Crear-Perry, “Root Causes of Black Maternal Health Inequities: Improving Access to Perinatal Care: Confronting Disparities & Inequities in Maternal-Infant Health,” National Birth Equity Collaborative (April 2019), 50.
- 13K. M. Hoffman et al., “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences between Blacks and Whites,” Proceedings of the National Academy of Sciences 113, no. 16 (April 19, 2016): 4296–4301.
- 14Kimberly Crenshaw, “Mapping the Margins,” Stanford Law Review 43, no. 6 (1991): 1241–99. https://doi.org/10.2307/1229039.
- 15Michael Omi and Howard Winant, Racial Formation in the United States (Routledge, 2014).
- 16We acknowledge that whiteness is a further societal construct that has changed drastically over time; however, a full critical analysis of whiteness is not the point of this essay and can be found elsewhere. See appendix for more.
- 17Michael Yudell et al., “Taking Race out of Human Genetics,” Science 351, no. 6273 (February 5, 2016): 564–65. https://doi.org/10.1126/science.aac4951; Gravlee, “How Race Becomes Biology.”
- 18Gravlee, “How Race Becomes Biology.”
- 19Jenna M. Norton et al., “Social Determinants of Racial Disparities in CKD,” Journal of the American Society of Nephrology 27, no. 9 (September 2016): 2576–95. https://doi.org/10.1681/ASN.2016010027.
- 20Yudell et al., “Taking Race Out of Human Genetics”; Norton, “Social Determinants of Racial Disparities in CKD.”
- 21Ibid.
- 22Andrea Smith, “Heteropatriarchy and the Three Pillars of White Supremacy,” Color of Violence, edited by INCITE! Women of Color Against Violence (Duke University Press, 2016), 66–73. https://doi.org/10.1215/9780822373445-007.
- 23For more context on Mauna Kea, see https://www.vox.com/identities/2019/7/24/20706930/mauna-kea-hawaii, among other journalistic sources.
- 24For more context on the Dakota Access Pipeline, see https://www.theguardian.com/us-news/video/2016/aug/29/north-dakota-oil-… and https://americanindian.si.edu/nk360/plains-treaties/dapl, among other journalistic sources.
- 25Many people, especially white people, may read this and believe it does not apply to them, nor to the world they see. It is not the job of this paper to convince you that white supremacy and racism exist. For those who are interested in dismantling white supremacy within themselves, we suggest finding local trainings or engaging with the Me and White Supremacy workbook written by Layla F. Saad.
- 26Alberta Civil Liberties Research Centre, “Racism and Power,” accessed March 1, 2020, http://www.aclrc.com/racism-and-power.
- 27The Aspen Institute: Roundtable on Community Change, “Glossary for Understanding the Dismantling Structural Racism/Promoting Racial Equity Analysis,” accessed March 1, 2020, https://assets.aspeninstitute.org/content/uploads/files/content/docs/rc….
- 28Alberta Civil Liberties Research Centre, “Forms of Racism,” accessed March 1, 2020, http://www.aclrc.com/forms-of-racism.
- 29Erin Digitale, “Microaggressions in Medical Training,” Scope (blog) (May 22, 2018), https://scopeblog.stanford.edu/2018/05/22/185969/.
- 30Derlad Wing Sue et al., “Racial Microaggressions in Everyday Life: Implications for Clinical Practice,” American Psychologist 62, no. 4 (2007): 271–86. https://doi.org/10.1037/0003-066X.62.4.271.
- 31Katie Johnston-Goodstar and Ross Roholt, “‘Our Kids Aren’t Dropping Out; They’re Being Pushed Out,’” Journal of Ethnic & Cultural Diversity in Social Work 26, no. 1–2 (January 2, 2017): 30–47. https://doi.org/10.1080/15313204.2016.1263818.
- 32Lucas Torres, Mark Driscoll, and Anthony Burrow, “Racial Microaggressions and Psychological Functioning Among Highly Achieving African-Americans,” Journal of Social and Clinical Psychology 29, no. 10 (December 1, 2010): 1074–99. https:// doi.org/10.1521/jscp.2010.29.10.1074; Kamaldeep Bhui, “The Impact of Racism on Mental Health,” Synergi Collaborative Centre (March 2018):14.; Kevin Nadal et al., “The Impact of Racial Microaggressions on Mental Health,” Journal of Counseling & Development 92, no. 1 (2014): 57–66. https://doi.org/10.1002/j.1556-6676.2014.00130.x; M. L. Walls et al., “Unconscious Biases,” Journal of the American Board of Family Medicine 28, no. 2 (March 1, 2015): 231–39.
- 33T. T. Lewis et al., “Chronic Exposure to Everyday Discrimination and Coronary Artery Calcification in African-American Women,” Psychosomatic Medicine 68, no. 3 (June 2006): 362–368. https://doi.org/10.1097/01.psy.0000221360.94700.16; Wendy Troxel et al., “Chronic Stress Burden, Discrimination, and Subclinical Carotid Artery Disease in African American and Caucasian Women,” Health Psychology 22, no. 3 (2003): 300–309. https://doi.org/10.1037/0278-6133.22.3.300; T. R. Taylor et al., “Racial Discrimination and Breast Cancer Incidence in US Black Women: The Black Women’s Health Study,” American Journal of Epidemiology 166, no. 1 (July 1, 2007): 46–54. https://doi.org/10.1093/aje/kwm056; Robert Edwards, “The Association of Perceived Discrimination with Low Back Pain,” Journal of Behavioral Medicine 31, no. 5 (October 2008): 379–89. https://doi.org/10.1007/s10865-008-9160-9; Mario Sims et al., “Perceived Discrimination and Hypertension Among African Americans in the Jackson Heart Study,” Journal of Behavioral Medicine 31, no. 5 (October 2008): 379–89. https://doi.org/10.1007/s10865-008-9160-9; David Williams and Selina Mohammed, “Racism and Health,” American Behavioral Scientist 57, no. 8 (August 1, 2013). https://doi.org/10.1177/0002764213487340.
- 34American Psychological Association, “Featured Commentary: Trayvon, Troy, Sean: When Racial Biases and Microaggressions Kill,” (July 2012), https://www.apa.org/pi/oema/resources/communique/2012/07/microaggressio….
- 35Alexis Johnson and Rachel Godsil, “The Science of Equality, Volume 1: Addressing Implicit Bias, Racial Anxiety, and Stereotype Threat in Education and Healthcare,” Perception Institute 1 (November 2014): 90.
- 36Donna Bivens, “Internalized Racism: A Definition,” Women’s Theological Center (1995).
- 37Carlos Hipolito-Delgado, “Exploring the Etiology of Ethnic Self-Hatred,” Chicana/o and Latina/o College Students,” Journal of College Student Development 51, no. 3 (May 23, 2010): 319–31. doi.org/10.1353/csd.0.0133.
- 38A&M, “Internalized Racism Among Asians,” Medium (October 14, 2018), https://medium.com/a-m-awaken-your-inner-asian/internalized-racism-amon….
- 39US News & World Report, “Rub Out the Bias Behind Skin-Lightening Products,” accessed March 3, 2020, https://www.usnews.com/news/best-countries/articles/2017-04-17/global-w…; Roger Lee Mendoza, “The Skin Whitening Industry in the Philippines,” Journal of Public Health Policy 35, no. 2 (May 1, 2014): 219–38. https://doi.org/10.1057/jphp.2013.50; Eric P. H. Li, Hyun Jeong Min and Russell Belk, “Skin Lightening and Beauty in Four Asian Cultures,” Association for Consumer Research, North American Advances 35 (2008), https:///www.acrwebsite.org/volumes/13415/volumes/v35/NA-35; Mohammed Adow, “Nigeria’s Dangerous Skin Whitening Obsession,” Al Jazeera (April 6, 2013), https://www.aljazeera.com/indepth/features/2013/04/20134514845907984.ht….
- 40Earle Chambers et al., “The Relationship of Internalized Racism to Body Fat Distribution and Insulin Resistance among African Adolescent Youth,” Journal of the National Medical Association 96, no. 12 (December 2004): 1594–98.; S. E. Tull et al., “Relationship of Internalized Racism to Abdominal Obesity and Blood Pressure in Afro-Caribbean Women,” Journal of the National Medical Association 91, no. 8 (August 1999): 447–52.
- 41Dee Watts‐Jones, “Healing Internalized Racism,” Family Process 41, no. 4 (2002): 591–601. https://doi.org/10.1111/j.1545-5300.2002.00591.x; Kira Hudson Banks and Jadah Stephens, “Reframing Internalized Racial Oppression and Charting a Way Forward,” Social Issues and Policy Review 12, no. 1 (2018): 91–111. https://doi.org/10.1111/sipr.12041.
- 42Sharon Brown et al., “Culturally Competent Diabetes Self-Management Education for Mexican Americans,” Diabetes Care 25, no. 2 (February 1, 2002): 259–68. https://doi.org/10.2337/diacare.25.2.259; Peter Zeh et al., “A Cross-Sectional Survey of General Practice Health Workers’ Perceptions of Their Provision of Culturally Competent Services to Ethnic Minority People with Diabetes,” Primary Care Diabetes 12, no. 6 (December 1, 2018): 501–9. https://doi.org/10.1016/j.pcd.2018.07.016.
- 43Juliene Lipson and Suzanne L. Dibble, eds., Culture & Nursing Care: A Pocket Guide (San Francisco: University of California, San Francisco, Nursing Press, 1996).
- 44Juliene Lipson and Suzanne L. Dibble, eds., Culture & Clinical Care (San Francisco: University of California, San Francisco, Nursing Press, 2005).
- 45Melanie Tervalon and Jann Murray-García, “Cultural Humility versus Cultural Competence,” Journal of Health Care for the Poor and Underserved 9, no. 2 (1998): 117–25. https://doi.org/10.1353/hpu.2010.0233.
- 46Frances Maurer and Claudia Smith, Community/Public Health Nursing Practice, 5th ed. (St. Louis, MO: Elsevier/Saunders, 2013); Marcia Stanhope and Jeanette Lancaster, Public Health Nursing. Health for Families and Populations, 5th ed. (St. Louis, MO: Elsevier/Saunders, 2013).
- 47Tervalon, “Cultural Humility versus Cultural Competence.”
- 48Maria Veronica Svetaz et al., “Racism and Its Harmful Effects on Nondominant Racial–Ethnic Youth and Youth-Serving Providers: A Call to Action for Organizational Change,” The Society for Adolescent Health and Medicine, Journal of Adolescent Health 63, no. 2 (August 1, 2018): 257–61. doi.org/10.1016/j.jadohealth.2018.06.003; Zinzi D. Baily et al., “Structural Racism and Health Inequities in the USA,” The Lancet 389, no. 10077 (April 8, 2017): 1453–63. https://doi.org/10.1016/S0140-6736(17)30569-X.
- 49Centers for Disease Control and Prevention, “Social Determinants of Health: Know What Affects Health,” accessed on February 20, 2019, https://www.cdc.gov/socialdeterminants/index.htm: Social determinants of health are “conditions in the places where people live, learn, work, and play, [which] affect a wide range of health risks and outcomes,” which leads to the call for a “creat[ion of] social and physical environments that promote good health for all.”
- 50Dorothy E. Roberts, Killing the Black Body: Race, Reproduction, and the Meaning of Liberty (New York: Vintage Books, 2014); Khiara Bridges, Reproducing Race: An Ethnography of Pregnancy as a Site of Racialization (Berkeley: University of California Press, 2011).
- 51 Tara O’Neill Hayes and Carly McNeil, “Maternal Mortality in the United States,” American Action Forum (September 9, 2019), https://www.americanactionforum.org/insight/maternal-mortality-in-the-u….
- 52Hayes, “Maternal Mortality in the United States.”
- 54Bailey, “Structural Racism and Health Inequities in the USA.”
- 55Jo C. Phelan, Bruce G. Link, and Parisa Tehranifar, “Social Conditions as Fundamental Causes of Health Inequalities,” Journal of Health and Social Behavior 51, no. 1 (March 2010): S28–40. https://doi.org/10.1177/0022146510383498.
- 56Bailey, “Structural Racism and Health Inequities in the USA.”
- 57Anthony Nardone et al., “Associations between Historical Residential Redlining and Current Age-Adjusted Rates of Emergency Department Visits Due to Asthma across Eight Cities in California,” The Lancet Planetary Health 4, no. 1 (January 1, 2020): e24–31. https://doi.org/10.1016/S2542-5196(19)30241-4.
- 58Bailey, “Structural Racism and Health Inequities in the USA.”
- 59Shauntice Allen et al., “The Search for Environmental Justice,” International Journal of Environmental Research and Public Health 16, no. 12 (June 14, 2019): 2117. https://doi.org/10.3390/ijerph16122117; David Kramar et al., “A Spatially Informed Analysis of Environmental Justice: Analyzing the Effects of Gerrymandering and the Proximity of Minority Populations to US Superfund Sites,” Environmental Justice 11, no. 1 (February 2018): 29–39. doi.org/10.1089/env.2017.0031; Chlore Reichel, “Toxic Waste Sites and Environmental Justice: Research Roundup,” Journalist’s Resource (blog) (September 24, 2018), https://journalistsresource.org/studies/environment/superfund-toxic-was….
- 60Omi, Racial Formation in the United States.
- 61Camila Hällgren and Gaby Weiner, “Out of the Shadow of Linnaeus: Acknowledging Their Existence and Seeking to Challenge, Racist Practices in Swedish Educational Settings” (2006), http://www.leeds.ac.uk/educol/documents/157423.htm.
- 62Stephen Jay Gould, The Mismeasure of Man (W. W. Norton & Company, 1996).
- 63David Hurst Thomas and Canby Jr., Skull Wars: Kennewick Man, Archaeology, and the Battle for Native American Identity (New York: Basic Books, 2001).
- 64Edwin Black, “Eugenics and the Nazis—the California Connection,” San Francisco Chronicle (November 9, 2003), https://www.sfgate.com/opinion/article/Eugenics-and-the-Nazis-the-Calif….
- 65Telford Taylor, “Trials of War Criminals before the Nuernberg Military Tribunals under Control Council Law No. 10,” Military Legal Resources (n.d.).
- 66Black, “Eugenics and the Nazis—the California Connection.”
- 67Black, “Eugenics and the Nazis—the California Connection.”
- 68The American College of Obstetricians and Gynecologists (@ACOGAction), “The answer is...B. #ACOG19 Bipolar disorder increases risk of suicide,” Twitter, May 4, 2019, https://twitter.com/acogaction/status/1124713954977165312.
- 69Aziza Sedrak and Noah Kondamudi, “Sickle Cell Disease,” StatPearls (November 18, 2019), https://www.statpearls.com/kb/viewarticle/29015.
- 70Vinay Kumar, Abul K. Abbas, and Jon C. Aster, Robbins and Cotran Pathologic Basis of Disease, 9th edition (Philadelphia, PA: Elsevier, 2014).
- 71Ben White, “How to Approach NBME/USMLE Questions,” (July 21, 2013), https://www.benwhite.com/medicine/how-to-approach-nbme-usmle-questions/.
- 72Kelsey Ripp and Lundy Braun, “Race/Ethnicity in Medical Education,” Teaching and Learning in Medicine 29, no. 2 (June 2017): 115–22. https://doi.org/10.1080/10401334.2016.1268056.
- 73Yudell et al., “Taking Race out of Human Genetics,” 564–65.
- 74Alicia Lukachko, Mark L. Hatzenbuehler, and Katherine M. Keyes, “Structural Racism and Myocardial Infarction in the United States,” Social Science & Medicine 103 (February 2014): 42–50. https://doi.org/10.1016/j.socscimed.2013.07.021.
- 75Gene H. Brody et al., “Perceived Discrimination among African American Adolescents and Allostatic Load,” Child Development 85, no. 3 (May 2014): 989–1002. https://doi.org/10.1111/cdev.12213.
- 76Lukachko, “Structural Racism and Myocardial Infarction in the United States.”
- 77Paul A. James et al., “2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee,” Journal of the American Medical Association 311, no. 5 (February 5, 2014): 507–20. https://doi.org/10.1001/jama.2013.284427.
- 78Stephan K. Williams et al., “Hypertension Treatment in Blacks: Discussion of the US Clinical Practice Guidelines,” Progress in Cardiovascular Diseases 59, no. 3 (2016): 282–88. https://doi.org/10.1016/j.pcad.2016.09.004.
- 79Heidi Lujan and Stephen DiCarlo, “The ‘African Gene’ Theory: It Is Time to Stop Teaching and Promoting the Slavery Hypertension Hypothesis,” Advances in Physiology Education 42, no. 3 (July 4, 2018): 412–16. https://doi.org/10.1152/advan.00070.2018.
- 80“High Blood Pressure in African-Americans: Genetics, Risks, Causes, and More,” WebMD, accessed March 1, 2020, https://www.webmd.com/hypertension-high-blood-pressure/guide/hypertensi….
- 81Lujan and DiCarlo, “The ‘African Gene’ Theory.”
- 82David Cutler, Roland G. Fryer, and Edward L. Glaeser, “Racial Differences in Life Expectancy: The Impact of Salt, Slavery, and Selection,” Unpublished Manuscript, Harvard University and the National Bureau of Economic Research, March 1, 2005.
- 83Cutler, Fryer, and Glaeser, “Racial Differences in Life Expectancy.”
- 84Stephen J. Dubner, “Toward a Unified Theory of Black America,” New York Times, sec. Magazine (March 20, 2005), https://www.nytimes.com/2005/03/20/magazine/toward-a-unified-theory-of-….
- 85Osagie K. Obasogie, “Oprah’s Unhealthy Mistake,” Los Angeles Times (May 17, 2007), https://www.latimes.com/archives/la-xpm-2007-may-17-oe-obasogie17-story….
- 86Ibid.
- 87Osagie K. Obasogie, “The Return of Biological Race? Regulating Race and Genetics Through Administrative Agency Race Impact Assessments,” Southern California Interdisciplinary Law Journal 22 (January 1, 2012): 1.
- 88Jonathan D. Kahn, “From Disparity to Difference: How Race-Specific Medicines May Undermine Policies to Address Inequalities in Health Care,” Southern California Interdisciplinary Law Journal 15, no. 1 (2005): 105–30.
- 89Ibid.
- 90Ibid.
- 91Obasogie, “The Return of Biological Race?”
- 92Ibid.
- 93Denise Gellene, “Heart Pill Intended Only for Blacks Sparks Debate,” Los Angeles Times (June 16, 2005).
- 94Ibid.
- 95Obasogie, “The Return of Biological Race?”
- 96Betram Katzung, Basic and Clinical Pharmacology, 14th edition (New York: McGraw-Hill Education/Medical, 2017).
- 97Dorothy E. Roberts, “What’s Wrong with Race-Based Medicine?” Faculty Scholarship at Penn Law (January 1, 2011), https://scholarship.law.upenn.edu/faculty_scholarship/435.
- 99Ibid.
- 100Ibid.
- 101Ibid; “How High Blood Pressure Can Lead to Kidney Damage or Failure,” American Heart Association, https://www.heart.org/en/health-topics/high-blood-pressure/health-threa….
- 102The American Heart Association describes the mechanism as “over time, uncontrolled high blood pressure can cause arteries around the kidneys to narrow, weaken or harden. These damaged arteries are not able to deliver enough blood to the kidney tissue.”
- 103National Kidney Foundation, “Frequently Asked Questions about GFR Estimates,” https://www.kidney.org/content/frequently-asked-questions-about-gfr-est….
- 104Ibid.
- 105Carmen Peralta et al., “Race Differences in Prevalence of Chronic Kidney Disease among Young Adults Using Creatinine-Based Glomerular Filtration Rate-Estimating Equations,” Nephrology Dialysis Transplantation 25, no. 12 (December 2010): 3934–39. https://doi.org/10.1093/ndt/gfq299.
- 106Nicholas, Kalantar-Zadeh, and Norris, “Racial Disparities in Kidney Disease Outcomes”; Wilkinson “Inequalities and Outcomes.”
- 107Peralta et al., “Race Differences in Prevalence of Chronic Kidney Disease.”
- 108Norton, “Social Determinants of Racial Disparities in CKD,” 2576–95.
- 109Ibid.
- 110National Kidney Foundation, “Frequently Asked Questions About GFR Estimates.”
- 111Juliana Zanocco et al., “Race Adjustment for Estimating Glomerular Filtration Rate Is Not Always Necessary,” Nephron Extra 2, no. 1 (January 2012): 293–302. https://doi.org/10.1159/000343899.
- 112Peralta, “Race Differences in Prevalence of Chronic Kidney Disease.”
- 113 Zanocco et al., “Race Adjustment for Estimating Glomerular Filtration Rate.”
- 114Andrew Levey et al., “A More Accurate Method to Estimate Glomerular Filtration Rate from Serum Creatinine: A New Prediction Equation. Modification of Diet in Renal Disease Study Group,” Annals of Internal Medicine 130, no. 6 (March 16, 1999): 461–70. https://doi.org/10.7326/0003-4819-130-6-199903160-00002.
- 115S. H. Cohn et al., “Body Elemental Composition Comparison between Black and White Adults,” American Journal of Physiology 232, no. 4 (April 1977): E419-422. https://doi.org/10.1152/ajpendo.1977.232.4.E419; David W. Harsha, Ralph R. Frerichs, and Gerald S. Berenson, “Densitometry and Anthropometry of Black and White Children,” Human Biology 50, no. 3 (1978): 261–80; J. G. Worrall et al., “Racial Variation in Serum Creatine Kinase Unrelated to Lean Body Mass,” British Journal of Rheumatology 29, no. 5 (October 1990): 371–73. https://doi.org/10.1093/rheumatology/29.5.371; Levey et al., “A More Accurate Method to Estimate Glomerular Filtration Rate.”
- 116Levey et al., “A New Equation to Estimate Glomerular Filtration Rate.”
- 117Zanocco et al., “Race Adjustment for Estimating Glomerular Filtration Rate Is Not Always Necessary.”
- 118Toni Martin, “The Color of Kidneys,” American Journal of Kidney Diseases 58, no. 5 (November 1, 2011): A27–28. https://doi.org/10.1053/j.ajkd.2011.08.018.
- 119National Kidney Foundation, “Frequently Asked Questions about GFR Estimates.”
- 120Andre Araujo et al., “Lean Mass, Muscle Strength, and Physical Function in a Diverse Population of Men,” BMC Public Health 10, no. 1 (August 21, 2010): 508. https://doi.org/10.1186/1471-2458-10-508; D. R. Wagner and V. H. Heyward, “Measures of Body Composition in Blacks and Whites,” American Journal of Clinical Nutrition 71, no. 6 (June 2000): 1392–1402. https://doi.org/10.1093/ajcn/71.6.1392; Analiza Silva et al., “Ethnicity-Related Skeletal Muscle Differences across the Lifespan,” American Journal of Human Biology 22, no. 1 (February 2010): 76–82. https://doi.org/10.1002/ajhb.20956.
- 121B. Hawkins, The New Plantation: Black Athletes, College Sports, and Predominantly White NCAA Institutions, (Palgrave Macmillan US, 2010). https://doi.org/10.1057/9780230105539.
- 122Roberts, “The Problem with Race-Based Medicine.”
- 123Martin, “The Color of Kidneys.”
- 124Martin, “The Color of Kidneys.”
- 125Lundy Braun, Breathing Race into the Machine: The Surprising Career of the Spirometer from Plantation to Genetics (Minneapolis: University of Minnesota Press, 2014).
- 126Ibid.
- 127Lundy Braun, “Race, Ethnicity and Lung Function,” Perspectives in Biology and Medicine 45, no. 2 (May 1, 2002): 159–74. https://doi.org/10.1353/pbm.2002.0023.
- 128Braun, Breathing Race into the Machine.
- 129Eleanor Bader, “Racializing Lung Function,” Truthout, accessed March 2, 2020, https://truthout.org/articles/racializing-lung-function/.
- 130Braun, Breathing Race into the Machine.
- 131Meredith C. McCormack, “Selecting Reference Values for Pulmonary Function Tests,” UpToDate (July 24, 2018), https://www-uptodate-com.ucsf.idm.oclc.org/contents/selecting-reference….
- 132John Hankinson, John Odencrantz, and Kathleen Fedan, “Spirometric Reference Values from a Sample of the General U.S. Population,” American Journal of Respiratory and Critical Care Medicine 159, no. 1 (January 1, 1999): 179–87. https://doi.org/10.1164/ajrccm.159.1.9712108.
- 133R. Pellegrino et al., “Interpretative Strategies for Lung Function Tests,” The European Respiratory Journal 26, no. 5 (November 2005): 948–68. https://doi.org/10.1183/09031936.05.00035205.
- 134Anne Fausto-Sterling, “I Can’t Breathe,” Boston Review (March 17, 2016), http://bostonreview.net/wonders/anne-fausto-sterling-race-medical-school.
- 135Erin Texeira, “Racial Basis for Asbestos Lawsuits?; Owens Corning Seeks More Stringent Standards for Blacks,” Baltimore Sun (March 25, 1999), https://www.baltimoresun.com/news/bs-xpm-1999-03-25-9903250041-story.ht….
- 136Bruce Culver et al., “Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement,” American Journal of Respiratory and Critical Care Medicine 196, no. 11 (December 2017): 1463–72. https://doi.org/10.1164/rccm.201710-1981ST.
- 137Philip Quanjer et al., “Multi-ethnic Reference Values for Spirometry for the 3-95 Year Age Range,” The European Respiratory Journal 40, no. 6 (December 2012): 1324–43. https://doi.org/10.1183/09031936.00080312.
- 138Hamza Shaban, “How Racism Creeps Into Medicine,” The Atlantic (August 29, 2014), https://www.theatlantic.com/health/archive/2014/08/how-racism-creeps-in….
- 139Braun, “Race, Ethnicity, and Health,” 159–74; Chou, “How Science and Genetics Are Reshaping the Race Debate of the 21st Century,” Science in the News (blog) (April 17, 2017), http://sitn.hms.harvard.edu/flash/2017/science-genetics-reshaping-race-….
- 140Rajesh Kumar et al., “Genetic Ancestry in Lung-Function Predictions,” New England Journal of Medicine 363, no. 4 (July 22, 2010): 321–30. https://doi.org/10.1056/NEJMoa0907897.
- 141Hankinson, Odencrantz, and Fedan, “Spirometric Reference Values”; Elizabeth Kiefer, Graham Hankinson, and John Barr, “Similar Relation of Age and Height to Lung Function Among Whites, African Americans, and Hispanics,” American Journal of Epidemiology 173, no. 4 (February 15, 2011): 376–87. https://doi.org/10.1093/aje/kwq417; Quanjer et al., “Multi-ethnic Reference Values for Spirometry”; MyLinh Duong et al., “Global Differences in Lung Function by Region (PURE): An International, Community-Based Prospective Study,” The Lancet Respiratory Medicine 1, no. 8 (October 1, 2013): 599–609; Chen et al., “Relationship between Lung Function and Metabolic Syndrome,” PLoS ONE 9, no. 10 (October 9, 2014). https://doi.org/10.1371/journal.pone.0108989; Ana Maria Menezes et al., “African Ancestry, Lung Function and the Effect of Genetics,” The European Respiratory Journal 45, no. 6 (June 2015): 1582–89. https://doi.org/10.1183/09031936.00112114.
- 142Menezes et al., “African Ancestry, Lung Function and the Effect of Genetics”; Quanjer et al., “Multi-ethnic Reference Values for Spirometry.”
- 143Kiefer, Hankinson, and Barr, “Similar Relation of Age and Height to Lung Function.”
- 144Katherine Drake, Joshua Galanter, and Esteban Buchard, “Race, Ethnicity and Social Class and the Complex Etiologies of Asthma,” Pharmacogenomics 9, no. 4 (April 2008): 453–62. https://doi.org/10.2217/14622416.9.4.453; Duana Fullwiley, “The Biologistical Construction of Race,” Pharmacogenomics 9, no. 4 (April 2008): 453–62. https://doi.org/10.2217/14622416.9.4.453.
- 145Michael McGeachie et al., “Whole Genome Prediction and Heritability of Childhood Asthma Phenotypes,” Immunity, Inflammation and Disease 4, no. 4 (November 28, 2016): 487–96. https://doi.org/10.1002/iid3.133.
- 146Margaret Parker et al., “Admixture Mapping Identifies a Quantitative Trait Locus Associated with FEV1/FVC in the COPDGene Study,” Genetic Epidemiology 38, no. 7 (November 2014): 652–59. https://doi.org/10.1002/gepi.21847.
- 147Yudell et al., “Taking Race out of Human Genetics.”
- 148Rajesh Kumar et al., “Genetic Ancestry in Lung-Function Predictions.”
- 149Yudell et al., “Taking Race out of Human Genetics.”
- 150Fullwiley, “The Biologistical Construction of Race”; Dorothy E. Roberts, “Is Race-Based Medicine Good for Us? African American Approaches to Race, Biomedicine, and Equality,” The Journal of Law, Medicine & Ethics (August 1, 2008). doi/10.1111/j.1748-720X.2008.302.x; Roberts, “The Problem with Race-Based Medicine”; Troy Duster, “Buried Alive,” in Genetic Nature/Culture: Anthropology and Science beyond the Two-Culture Divide,edited by Alan H. Goodman, Deborah Heath, and M. Susan Lindee, 258–77 (University of California Press, 2003). www.jstor.org/stable/10.1525/j.ctt1pp2bv.19; Troy Duster, “Race and Reification in Science,” Science 307, no. 5712 (February 18, 2005): 1050–51. https://doi.org/10.1126/science.1110303.
- 151See, for example, Ian Holmes, “David Reich, Racism, and the Difficulty of Talking About Genetics, ” The Atlantic, https://www.theatlantic.com/science/archive/2018/04/reich-genetics-raci….
- 152Neha John-Henderson et al., “Socioeconomic Status and Social Support: Social Support Reduces Inflammatory Reactivity for Individuals Whose Early-Life Socioeconomic Status Was Low,” Psychological Science 26, no. 10 (October 1, 2015): 1620–29. https://doi.org/10.1177/095679761559596.
- 153Lawrence Wallack and Kent Thornburg, “Developmental Origins, Epigenetics, and Equity,” Maternal and Child Health Journal 20, no. 5 (May 1, 2016): 935–40. https://doi.org/10.1007/s10995-016-1970-8; Christopher Kuzawa and Elizabeth Sweet, “Epigenetics and the Embodiment of Race: Developmental Origins of US Racial Disparities in Cardiovascular Health,” American Journal of Human Biology 21, no. 1 (2009): 2–15. https://doi.org/10.1002/ajhb.20822.
- 154Robert-Paul Juster et al., “Allostatic Load and Comorbidities: A Mitochondrial, Epigenetic, and Evolutionary Perspective,” Development and Psychopathology 28, no. 4pt1 (2016): 1117–46. https://doi.org/10.1017/S0954579416000730.
- 155Laura Richman and Charles Jonassaint, “The Effects of Race-Related Stress on Cortisol Reactivity in the Laboratory: Implications of the Duke Lacrosse Scandal,” Annals of Behavioral Medicine 35, no. 1 (February 1, 2008): 105–10. https://doi.org/10.1007/s12160-007-9013-8.
- 156Pamela Sawyer et al., “Discrimination and the Stress Response: Psychological and Physiological Consequences of Anticipating Prejudice in Interethnic Interactions,” American Journal of Public Health 102, no. 5 (March 15, 2012): 1020–26. https://doi.org/10.2105/AJPH.2011.300620.
- 157Amani Nuru-Jeter et al., “Abstract 9550: Anticipatory Racism Threat and Superwoman Schema: Elucidating the Relationship Between Racial Discrimination and Chronic Inflammation,” Circulation 128, no. 22 (November 26, 2013): A9550–A9550. https://doi.org/10.1161/circ.128.suppl_22.A9550.
- 158Shannon Sullivan, “Inheriting Racist Disparities in Health: Epigenetics and the Transgenerational Effects of White Racism,” Critical Philosophy of Race 1, no. 2 (September 5, 2013): 190–218.
- 159Kuzawa and Sweet, “Epigenetics and the Embodiment of Race”; Sullivan, “Inheriting Racist Disparities in Health”; Wallack and Thornburg, “Developmental Origins, Epigenetics, and Equity”; Darlene Francis, “Conceptualizing Child Health Disparities: A Role for Developmental Neurogenomics,” Pediatrics 124, no. 3 (November 2009): 196–202. https://doi.org/10.1542/peds.2009-1100G.
- 160Francis, “Conceptualizing Child Health Disparities.”
- 161Kuzawa and Sweet, “Epigenetics and the Embodiment of Race.”
- 162Francis, “Conceptualizing Child Health Disparities.”
- 163 Sullivan, “Inheriting Racist Disparities in Health.”